Abstract
Case Report
Prostate health in India (BPH & Prostate Cancer)
Suresh Kishanrao*
Published: 03 September, 2022 | Volume 6 - Issue 1 | Pages: 009-017
The prostate gland, found only in men, is an extremely important organ of the reproductive system, but it is not taken care of adequately, leading to prostate inflammation and benign hypertrophy or even cancer. Benign prostate enlargement compresses urine flow through the urethra, leading to uncomfortable urinary symptoms. Hyperplasia increases the risk of bladder stones, urinary tract infections, and kidney problems. In India prevalence of Benign Prostrate Hyperplasia (BPH) is around 50% of men by the age of 60 years. Studies suggest that benign prostatic hyperplasia is a result of the disproportion between oestrogen & testosterone. A higher proportion of oestrogen within the prostate boosts the growth of prostate cells. The management of BPH is streamlined in recent times and the majority are on medical treatment.
Prostate cancers are one of the cancers showing a significant increase in incidence along with mouth and kidney and lung cancers among the male population. With an estimated population of 1400 million and about 98 million males over 50 years of age in mid-2022 and the average life expectancy increasing 68.4 years, has a bearing on the changing incidence and pattern of prostate cancer in the current decade in India. Based on the five population-based cancer registries in 2009-10, the age-adjusted annual incidence rates per lakh population of prostate cancers were highest in Delhi (10.2) followed by Bengaluru (8.7), Mumbai (7.3), Chennai (7) and Bhopal (6.1). Cancer can co-exist with BPH. Prostate cancer management is still in the development stage with a 5-year life expectancy of around 64%.
The prostate is the second leading site of cancer among males in large Indian cities like Delhi, Kolkata, Pune, and Thiruvananthapuram, and the third leading site of cancer in cities like Bangalore and Mumbai. Despite the limitations of diagnosis, the annual cancer incidence rate ranges from 5.0-9.1 per 100,000/year, as compared to the rates in the United States and other developed countries of 110 &180 for whites and blacks respectively.
This article is a review of Prostate health in India based on a personal observation of around 183 cases by the author in the last 10 years.
Materials & methods: This is an observational study report of three cohorts of men across the country. The sample was of people encountering the author. The sample included i) 69 septuagenarians plus ii) 30 senior citizens aged 60 - 70 years and iii) 84 men in 40 – 60 - year age groups over the last decade. The data source was sharing annual check-up reports or consultation report in person for seeking 2nd opinion. A minimum of 2 consultations, first when diagnosed and the recent between July 2021 to June 2022.
Read Full Article HTML DOI: 10.29328/journal.acst.1001028 Cite this Article Read Full Article PDF
Keywords:
Prostate gland; Benign Prostate Hyperplasia (BPH); Cancer of Prostate (CAP); Cancer registries; Ultrasound (KUB); Prostate-Specific Antigen (PSA); Alpha-blockers; 5 alpha-reductase inhibitors & Transurethral Resection of the Prostate (TURP); Chemotherapy and Hormonal therapy
References
- Bhat SA, Rather SA, Islam N. An overview of benign prostatic hyperplasia and its appreciation in Greco-Arab (Unani) system of medicine. Asian J Urol. 2022 Apr;9(2):109-118. doi: 10.1016/j.ajur.2021.05.008. Epub 2021 May 29. PMID: 35509487; PMCID: PMC9051355.
- McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, Lepor H, McVary KT, Nyberg LM Jr, Clarke HS, Crawford ED, Diokno A, Foley JP, Foster HE, Jacobs SC, Kaplan SA, Kreder KJ, Lieber MM, Lucia MS, Miller GJ, Menon M, Milam DF, Ramsdell JW, Schenkman NS, Slawin KM, Smith JA; Medical Therapy of Prostatic Symptoms (MTOPS) Research Group. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003 Dec 18;349(25):2387-98. doi: 10.1056/NEJMoa030656. PMID: 14681504.
- Hariharan K, Padmanabha V. Demography and disease characteristics of prostate cancer in India. Indian J Urol. 2016 Apr-Jun;32(2):103-8. doi: 10.4103/0970-1591.174774. PMID: 27127351; PMCID: PMC4831497.
- Jain S. Epidemiology of prostate cancer in India. December 2014Meta Gene 2(C):596-605.
- Hashmi A. Prostate Cancer Cases Are Growing More Serious. https://www.medscape.com/viewarticle, 07 July, 2022
- Prostate enlargement. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases
- Thakur V, Singh PP, Talwar M, Mukherjee U. Utility of free/total prostate specific antigen (f/t PSA) ratio in diagnosis of prostate carcinoma. Dis Markers. 2003-2004;19(6):287-92. doi: 10.1155/2004/913870. PMID: 15258330; PMCID: PMC3851065.
- Malati T. Prostate specific antigen in patients of normal, benign prostate hypertrophy and carcinoma prostate. Indian J Clin Biochem. 2006; 21:34–40.
- Treatment of Benign prostate enlargement. https://www.nhs.uk/ conditions/ prostate-enlargement/treatment/
- Harinarayan CV, Holick MF, Prasad UV, Vani PS, Himabindu G. Vitamin D status and sun exposure in India. Dermatoendocrinol. 2013 Jan 1;5(1):130-41. doi: 10.4161/derm.23873. PMID: 24494046; PMCID: PMC3897581.
- Enlarged prostate diet: Foods to eat and avoid. https://www.medicalnewstoday.com/articles/321079
- Masturbation Frequency Linked to Prostate Risk in 20s, Protection in 50s. By Daniel J. DeNoon, medically Reviewed by Louise Chang, MD 27 January 2009, https://www.webmd.com/prostate-cancer/news/20090127
- Can Sex, Masturbation Affect Prostate Cancer Risk? R. Morgan Griffin and Medically Reviewed by Dany Paul Baby, MD on 22 April 2022, https://www.webmd.com/prostate-cancer/
- McVary KT. Management of benign prostatic hyperplasia (BPH). American Urological Association. https://www.auanet.org/guidelines/ 25 Sept. 2017
- Alvarez M. Can enlarged prostate shrink itself? https://www.quora.com/
Figures:
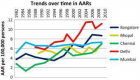
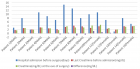
Figure 1
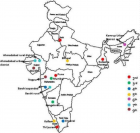
Figure 2
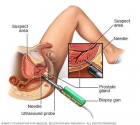
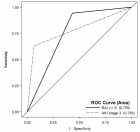
Figure 3
Similar Articles
-
Prostate health in India (BPH & Prostate Cancer)Suresh Kishanrao*. Prostate health in India (BPH & Prostate Cancer). . 2022 doi: 10.29328/journal.acst.1001028; 6: 009-017
Recently Viewed
-
Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary SurveyFatimah M Kaabi,Layth Mula-Hussain*,Shakir Al-Shakir,Sultan Alsaiari,Leonidas Chelis,Renda AlHabib,Sara Owaidah,Renad Subaie,Marwah M Abdulkader,Ibrahim Alotain. Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary Survey. Arch Cancer Sci Ther. 2026: doi: 10.29328/journal.acst.1001048; 10: 001-005
-
Screening for Depressive Symptoms in Clinical and Nonclinical Youth: The Psychometric Properties of the Dutch Children’s Depression Inventory-2 (CDI-2)Denise HM Bodden*,Yvonne Stikkelbroek,Daan Creemers,Sanne PA Rasing,Elien De Caluwe,Caroline Braet. Screening for Depressive Symptoms in Clinical and Nonclinical Youth: The Psychometric Properties of the Dutch Children’s Depression Inventory-2 (CDI-2). Insights Depress Anxiety. 2025: doi: 10.29328/journal.ida.1001047; 9: 028-039
-
Penile Fracture: The “Cracking” Sound and Intra-operative Tunica Albuginea RepairAyoub Mamad*,Mohammed Amine Bibat,Mohammed Amine Elafari,Youssef Maachi,Amine Slaoui,Tarik Karmouni,Abdelatif Koutani,Khalid Elkhader. Penile Fracture: The “Cracking” Sound and Intra-operative Tunica Albuginea Repair. J Clin Med Exp Images. 2026: doi: 10.29328/journal.jcmei.1001038; 10: 001-002
-
Transumbilical Single-incision Hiatal Hernia Repair and Nissen Fundoplication in situs Inversus Totalis: A Rare Case ReportQing Cao,Chen Kang,Kang Gu,Yin Peng,Yang Lv,Xu-Zhong Ding,Peng Li*. Transumbilical Single-incision Hiatal Hernia Repair and Nissen Fundoplication in situs Inversus Totalis: A Rare Case Report. Adv Treat ENT Disord. 2026: doi: 10.29328/journal.ated.1001017; 10: 001-003
-
NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and MuscleRizwan Uppal,Umar Saeed*,Muhammad Rehan Uppal. NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and Muscle. Ann Clin Endocrinol Metabol. 2026: doi: 10.29328/journal.acem.1001032; 10: 001-009
Most Viewed
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037
-
Snow white: an allergic girl?Oreste Vittore Brenna*. Snow white: an allergic girl?. Arch Asthma Allergy Immunol. 2022 doi: 10.29328/journal.aaai.1001029; 6: 001-002
-
Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disordersElena Viktorovna Drozdova*. Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disorders. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001028; 5: 038-040

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."