Abstract
Research Article
Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary Survey
Fatimah M Kaabi, Layth Mula-Hussain*, Shakir Al-Shakir, Sultan Alsaiari, Leonidas Chelis, Renda AlHabib, Sara Owaidah, Renad Subaie, Marwah M Abdulkader and Ibrahim Alotain
Published: 30 January, 2026 | Volume 10 - Issue 1 | Pages: 001-005
Background: WHO grade II Low-grade gliomas (LGGs) need multi-disciplinary treatment from different specialties, directed by new molecular classifications and prognostic markers. Yet regional practice patterns and obstacles are not reported, especially in MENA countries.
Method: A cross-sectional survey of physicians from MENA countries (including neurosurgeons, radiation oncologists, and medical oncologists) was conducted. An electronic anonymous survey, including clinical scenarios and evidence-based treatment choices, was distributed at professional conferences. The feedback included responses regarding surgical interventions, adjuvant treatment preferences, and barriers to adoption of IDH-mutant inhibitors.
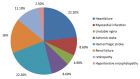
Results: 137 physicians (37.23% neurosurgery, 32.85% radiation oncology, 29.93% medical oncology). Most had 6–15 years of experience (56.21%) and worked in government (51.82%) or academic hospitals (25.55%). Maximal safe resection (MSR), if applicable, was preferred over biopsy (89.05% vs. 10.95%). For residual Astrocytoma, concurrent radiotherapy (RT) with temozolomide (TMZ) (42.34%) was the preferred adjuvant, while 44.53% prefer observation after gross total resection (GTR). For residual Oligodendroglioma, RT followed by PCV (45.99%) was preferred, with 59.85% offered observation post-GTR. Most (96.35%) agreed that resection extent impacts outcomes, while 72.99% objected to extending TMZ beyond six cycles. High-risk stratification varied: 46.72% used age ≥40 years, and 88.32% prioritized residual tumor volume. Although 64.96% supported IDH-mutant inhibitors, 58.39% cited limited availability as a barrier, followed by cost (40.88%) and insufficient long-term data (31.39%). Specialty-specific differences emerged: radiation oncologists tend more to provide adjuvant radiotherapy in the context of persistent seizure post-operatively (χ² = 20.50, p < 0.05), and medical/radiation oncologists more often used age ≥40 for high-risk stratification (χ² = 10.10, p = 0.038).
Conclusion: There is a wide variation in the WHO grade II LGGs management among physicians in MENA Countries. These data highlight the importance of locally derived guidelines, the increased availability of molecularly directed therapies, and ongoing collaboration between multiple disciplines to ensure optimal patient outcomes.
Key points:
• Maximal safe resection (89.05%) is the dominant surgical approach for WHO grade II LGGs, taking into consideration the location and extent of infiltration, among specialists in MENA Countries, reflecting global consensus on resection extent impacting outcomes (96.35% agreement).
• Adjuvant therapy preferences vary: concurrent RT+TMZ for astrocytomas (42.34%) and sequential RT+PCV for oligodendrogliomas (45.99%), with 59.85% observing post-GTR in oligodendrogliomas.
• IDH-mutant inhibitors (e.g., Vorasidenib) are supported by 64.96% of oncologists, but limited availability (58.39%) and cost (40.88%) hinder adoption.
Importance of the study: This multicenter survey is the first to evaluate real-world management trends and barriers for WHO grade II low-grade gliomas (LGGs) among physicians in MENA Countries. While all specialists align with international guidelines in surgical strategies (e.g., maximal safe resection), significant heterogeneity exists in adjuvant therapy choices, particularly for astrocytomas versus oligodendrogliomas. Crucially, we identify systemic barriers—such as limited access to molecular therapies (IDH inhibitors) and cost constraints—that disproportionately affect WHO grade II LGGs care in the MENA Countries. Our findings underscore the urgent need for regionally adapted guidelines and multidisciplinary collaboration to standardize practices aligned with international guidelines. By highlighting disparities in resource availability and specialty-specific decision-making (e.g., radiation oncologists prioritizing post-resection seizures, p < 0.05), this study provides a roadmap for optimizing WHO grade II LGGs management in resource-limited settings and advocates for the inclusion of Arab populations in global trials of novel agents like Vorasidenib.
Read Full Article HTML DOI: 10.29328/journal.acst.1001048 Cite this Article Read Full Article PDF
Keywords:
Low-grade glioma; IDH; Vorasidenib; Temozolomide
References
- Kratzsch T, Gautschi OP, Kuhn SA, Hottinger AF, Hildebrandt G, Stienen MN. Niedrig-gradige Gliome im Erwachsenenalter [Low-grade gliomas in adults]. Praxis (Bern 1994). 2014;103(23):1385–1396. German. Available from: https://doi.org/10.1024/1661-8157/a001835
- Chammas M, Saadeh F, Maaliki M, Assi H. Therapeutic interventions in adult low-grade gliomas. J Clin Neurol. 2019;15(1):1–8. Available from: https://doi.org/10.3988/jcn.2019.15.1.1
- Buckner JC, Pugh SL, Shaw EG, Gilbert MR, Barger G, Coons S, et al. Phase III study of radiation therapy with or without procarbazine, CCNU, and vincristine in low-grade glioma: RTOG 9802 with Alliance, ECOG, and SWOG. J Clin Oncol. 2014;32:15.
- Medical Research Council Brain Tumor Working Party. Randomized trial of procarbazine, lomustine, and vincristine in the adjuvant treatment of high-grade astrocytoma: a Medical Research Council trial. J Clin Oncol. 2001;19(2):509–518. Available from: https://doi.org/10.1200/jco.2001.19.2.509
- Jungk C, Gramatzki D, Trong PD, von Deimling A, Unterberg A. Revisiting the Pignatti risk score in low-grade glioma patients in the molecular era: NCOG-25. Neuro Oncol. 2021;23. Available from: https://doi.org/10.1093/neuonc/noab196.616
- van den Bent MJ, French PJ, Brat D, Tonn JC, Touat M, Ellingson BM, et al. The biological significance of tumor grade, age, enhancement, and extent of resection in IDH-mutant gliomas: how should they inform treatment decisions in the era of IDH inhibitors? Neuro Oncol. 2024;26(10):1805–1822. Available from: https://doi.org/10.1093/neuonc/noae107
- Mohile NA, Messersmith H, Gatson NT, Hottinger AF, Lassman A, Morton J, et al. Therapy for diffuse astrocytic and oligodendroglial tumors in adults: ASCO-SNO guideline. J Clin Oncol. 2022;40(4):403–426. Available from: https://doi.org/10.1200/jco.21.02036
- Buckner JC, Shaw EG, Pugh SL, Chakravarti A, Gilbert MR, Barger GR, et al. Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med. 2016;374(14):1344–1355. Available from: https://doi.org/10.1056/nejmoa1500925
- Mula-Hussain L, Mahdi H, Ramzi ZS, Tolba M, Zaghloul MS, Benbrahim Z, et al. Cancer burden among Arab world males in 2020: the need for a better approach to improve outcome. JCO Glob Oncol. 2022;(8):e2100407. Available from: https://doi.org/10.1200/go.21.00407
- Mahdi H, Mula-Hussain L, Ramzi ZS, Tolba M, Abdel-Rahman O, Abu-Gheida I, et al. Cancer burden among Arab-world females in 2020: working toward improving outcomes. JCO Glob Oncol. 2022;(8):e2100415. Available from: https://doi.org/10.1200/go.21.00415
- Houillier C, Wang X, Kaloshi G, Mokhtari K, Guillevin R, Laffaire J, Paris S, et al. IDH1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology. 2010;75(17):1560–1566. Available from: https://doi.org/10.1212/wnl.0b013e3181f96282
- Wijnenga MMJ, French PJ, Dubbink HJ, Dinjens WNM, Atmodimedjo PN, Kros JM, et al. The impact of surgery in molecularly defined low-grade glioma: an integrated clinical, radiological, and molecular analysis. Neuro Oncol. 2018;20(1):103–112. Available from: https://doi.org/10.1093/neuonc/nox176
- Xia L, Fang C, Chen G, Sun C. Relationship between the extent of resection and the survival of patients with low-grade gliomas: a systematic review and meta-analysis. BMC Cancer. 2018. Available from: https://doi.org/10.1186/s12885-017-3909-x
- Weller M, van den Bent M, Preusser M, Le Rhun E, Tonn JC, Minniti G, et al. Author correction: EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol. 2022;19(5):357–358. Available from: https://doi.org/10.1038/s41571-020-00447-z
- Minniti G, Paolini S, Antonelli M, Gianno F, Tini P, Lanzetta G, Arcella A, et al. Long-term treatment outcomes of temozolomide-based chemoradiation in patients with adult-type diffuse IDH-mutant grade 2 astrocytoma. J Neurooncol. 2023;164(2):331–339. Available from: https://doi.org/10.1007/s11060-023-04418-z
- Mellinghoff IK, van den Bent MJ, Blumenthal DT, Touat M, Peters KB, Clarke J, Mendez J, et al.; INDIGO Trial Investigators. Vorasidenib in IDH1- or IDH2-mutant low-grade glioma. N Engl J Med. 2023. Available from: https://doi.org/10.1056/nejmoa2304194
- Brown TJ, Bota DA, van den Bent MJ, Brown PD, Maher E, Aregawi D, et al. Management of low-grade glioma: a systematic review and meta-analysis. Neurooncol Pract. 2019;6(4):249–258. Available from: https://doi.org/10.1093/nop/npy034
- Jiang T, Nam DH, Ram Z, Poon WS, Wang J, Boldbaatar D, et al. Clinical practice guidelines for the management of adult diffuse gliomas. Cancer Lett. 2021;499. Available from: https://doi.org/10.1016/j.canlet.2020.10.050
Figures:
Similar Articles
-
Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary SurveyFatimah M Kaabi,Layth Mula-Hussain*,Shakir Al-Shakir,Sultan Alsaiari,Leonidas Chelis,Renda AlHabib,Sara Owaidah,Renad Subaie,Marwah M Abdulkader,Ibrahim Alotain. Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary Survey. . 2026 doi: 10.29328/journal.acst.1001048; 10: 001-005
Recently Viewed
-
Knowledge, Attitude, and Practices of Parents toward (Infant & Child) Oral Health in Family Medicine Center at PSMMC, RiyadhMaryam Alanazi*, Wed Alanazi, Hanan Alali, Fatma Alnoaimi, Arwa Shuwaykan, Nuha Al-Yahya. Knowledge, Attitude, and Practices of Parents toward (Infant & Child) Oral Health in Family Medicine Center at PSMMC, Riyadh. J Oral Health Craniofac Sci. 2023: doi: 10.29328/journal.johcs.1001044; 8: 016-023
-
Success, Survival and Prognostic Factors in Implant Prosthesis: Experimental StudyEpifania Ettore*, Pietrantonio Maria, Christian Nunziata, Ausiello Pietro. Success, Survival and Prognostic Factors in Implant Prosthesis: Experimental Study. J Oral Health Craniofac Sci. 2023: doi: 10.29328/journal.johcs.1001045; 8: 024-028
-
A Resurgence of the Idea of Hypertriglyceridemia and Lower Serum (HDL-C) as Predictive Factors for Insulin Resistance (IR) & Type 2 Diabetes Mellitus Development: A Narrative ReviewKulvinder Kochar Kaur*. A Resurgence of the Idea of Hypertriglyceridemia and Lower Serum (HDL-C) as Predictive Factors for Insulin Resistance (IR) & Type 2 Diabetes Mellitus Development: A Narrative Review. New Insights Obes Gene Beyond. 2025: doi: 10.29328/journal.niogb.1001022; 9: 001-012
-
Novel Mutation in Famous Gene Diseases in Red Blood CellsMahdi Nowroozi*. Novel Mutation in Famous Gene Diseases in Red Blood Cells. New Insights Obes Gene Beyond. 2025: doi: 10.29328/journal.niogb.1001023; 9: 013-020
-
Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical TrialAnders Wänman*, Susanna Marklund, Negin Yekkalam. Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical Trial. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001046; 9: 001-008
Most Viewed
-
Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trialSathit Niramitmahapanya*,Preeyapat Chattieng,Tiersidh Nasomphan,Korbtham Sathirakul. Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trial. Ann Clin Endocrinol Metabol. 2023 doi: 10.29328/journal.acem.1001026; 7: 00-007
-
Physical Performance in the Overweight/Obesity Children Evaluation and RehabilitationCristina Popescu, Mircea-Sebastian Șerbănescu, Gigi Calin*, Magdalena Rodica Trăistaru. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001030; 8: 004-012
-
Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging PresentationKarthik Baburaj*, Priya Thottiyil Nair, Abeed Hussain, Vimal MV. Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging Presentation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001029; 8: 001-003
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023 doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The benefits of biochemical bone markersSek Aksaranugraha*. The benefits of biochemical bone markers. Int J Bone Marrow Res. 2020 doi: 10.29328/journal.ijbmr.1001013; 3: 027-031

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."