More Information
Submitted: 11 April 2020 | Approved: 22 April 2020 | Published: 23 April 2020
How to cite this article: Machado MT, Taha A. Minimally invasive gracilis muscle transposition: Initial report. Arch Cancer Sci Ther. 2020; 4: 017-018.
DOI: 10.29328/journal.acst.1001016
Copyright License: © 2020 Machado MT, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Gracilis muscle; Urinary fistula; Minimally invasive surgery
Minimally invasive gracilis muscle transposition: Initial report
Tobias Machado* and Anis Taha
ABC Medical School, Santo André & Dr. Arnaldo Vieira de Carvalho Cancer Institute, San Paulo, Brazil
*Address for Correspondence: Marcos Tobias Machado, MD, Department of Urology, Centro Universitário Saúde 20 ABC, Av. Lauro Gomes, 2000 - Vila Sacadura Cabral, Santo André, SP, Brazil, 09060-870, Email: [email protected]
Rectourethral fistula (RUF) is a divesting complication after prostate cancer treatment. The RUF incidence after radical prostatectomy is about 0.5% to 2%, [1,2]. Radiotherapy, criotherapy and high intensity focused ultrasound are other more severe causes [3,4].
Repair of RUF is a challenging surgical procedure. There are some possible approaches but transperineal is the most utilized.
In cases of complex fistulas interposition of muscle flaps between the rectum and urethra is highly recommended. Gracilis muscle transposition (GMT) is the preferred, due to excellent mobility and vascularization for perineal reconstruction [5,6]. Dissection of the gracilis muscle is done using one, 2 or 3 large incisions in the medial border of the thigh.
The aim of this report is present a new minimally invasive access to obtain a pediculate flap of gracilis muscle to interposition between bladder and rectum to treat RUF.
A 60 years old male submitted to radical prostatectomy for prostatic adenocarcinoma present RUF postoperatively. Fecal diversion and 2 attempt of perineal and abdominal repairs were performed without success in other center. Cistoscopic evaluation reveal 1.5cm RUF with ischaemic borders at anastomotic area. We plan to perform an initial perineal approach with repair and interposition of gracilis muscle. If necessary abdominal approach combined to perineal dissection will be done.
Surgical technique
We idealize and perform successfully a new technique throught a small incision utilizing laparoscopic matherial following this 10 standardized steps:
1) After perineal approach and RUF repair, external rotation and abduction of left limb was performed.
2) Identification by palpation of the gracilis muscle and its distal tendon, differentiation of the rest of the muscular structures.
3) Incision 2.5 cm medial to knee joint above the gracilis insertion tendon.
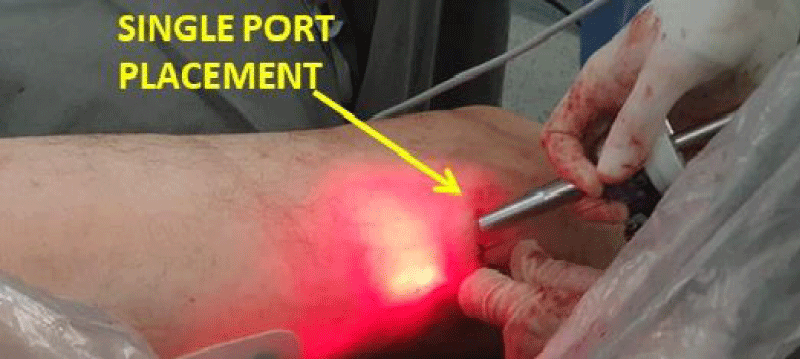
4) Blunt finger dissection for laparoscopic single port placement or two regular trocars (5 mm and 10 mm) (Figure 1).
Figure 1: 2.5cm incision at gracilis tendon area to Single Port placement.
5) Insufflation of Co2 (10-15 mmHg) to achieve working space.
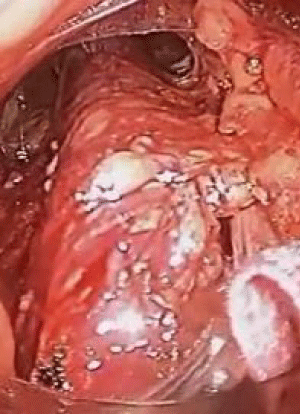
6) Complete dissection of the muscle is performed from its distal portion to its proximal portion preserving its main pedicle (Figure 2).
Figure 2: Endoscopic view of dissected gracilis muscle.
7) Cut of the distal tendon of the gracilis.
8) Transposition of the distal portion of the gracilis muscle through the subcutaneous tunnel to the perineal region.
9) Interposition of the muscle flap between the urethra and the rectum at least 3 cm above the fistula.
10) Fixation of gracilis with absorbable suture.
Operative time was 60 min, no complications was observed and discharge occurred at first post-operative day. At 6 months of follow up no recurrence of RUF was obtained.
Gracilis muscle is utilized as interposition tissue for repair of genitourinary fistulas [5].
Classical access to obtain gracilis is open approach with large and few aesthetic incisions [5,6].
With this new technique gracilis muscle could be endoscopically dissected offering minimal pain and postoperative scar, with excellent functional and cosmetic results.
This initial experience was exploratory but results was promising.
As a new option of dissection, there are no comparative data besides our clinical impression based in this first case. It seems an easy and fast procedure, offering few pain and the smaller incision than previously described at literature.
In conclusion minimally invasive gracilis muscle dissection was feasible and safe with potential benefits. However, further studies with large number of patients with longer follow-up will be necessary to answer if this new surgery will have some application in urological armamentarium.
- Mandel P, Linnemannstons A, Chun F, Schlomm T, Pompe R, et al. Incidence, Risk Factors, Management, and Complications of Rectal Injuries During Radical Prostatectomy. Eur Urol Focus. 2018;4: 554-557. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/28753847
- Hechenbleikner EM, Buckley JC, Wick EC. Acquired rectourethral fistulas in adults: a systematic review of surgical repair techniques and outcomes. Dis Colon Rectum. 2013; 56: 374-383. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/23392154
- Hanna JM, Turley R, Castleberry A, Hopkins T, Peterson AC, et al. Surgical management of complex rectourethral fistulas in irradiated and nonirradiated patients. Dis Colon Rectum. 2014;57: 1105-1112. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25101607
- Chen S, Gao R, Li H, Wang K. Management of acquired rectourethral fistulas in adults. Asian J Urol. 2018; 5: 149-154. Pubmed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6032817/
- Korsun S, Liebig-Hoerl G, Fuerst A. Gracilis muscle transposition for treatment of recurrent anovaginal, rectovaginal, rectourethral, and pouch-vaginal fistulas in patients with inflammatory bowel disease. Tech Coloproctol. 2019; 23: 43-52. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/30604248
- Hotouras A, Ribas Y, Zakeri S, Murphy J, Bhan C, et al. Gracilis muscle interposition for rectovaginal and anovaginal fistula repair: a systematic literature review. Colorectal Dis. 2015; 17: 104-110. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25284745