More Information
Submitted: 18 May 2020 | Approved: 22 May 2020 | Published: 25 May 2020
How to cite this article: PLalya I, Laatitioui S, Essadi I, El Omrani A Khouchani M. Vaginal embryonal rhabdomyosarcoma in young woman: A case report and literature review. Arch Cancer Sci Ther. 2020; 4: 034-037.
DOI: 10.29328/journal.acst.1001020
ORCiD: orcid.org/0000-0002-2046-000X
Copyright License: © 2020 Lalya I, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Embryonal rhabdomyosarcoma; Vagina; Young woman
Vaginal embryonal rhabdomyosarcoma in young woman: A case report and literature review
Issam Lalya1*, Sana Laatitioui1, Ismail Essadi2, Abdelhamid E1 Omrani1 and Mouna Khouchani1
1Department of Radiation Oncology, Mohammed VI Oncology Hematology Center, Cadi Ayyad University, Marrakesh, Morocco
2Department of Medical Oncology, Military Teaching Hospital Avicenne, Cadi Ayyad University, Marrakesh, Morocco
*Address for Correspondence: Issam Lalya, Department of Radiation Oncology, Mohammed VI Oncology Hematology Center, Cadi Ayyad University, Marrakesh, Morocco, Tel: 00212661572770; Email: [email protected]
Rhabdomyosarcomas are the most common soft tissue tumors of childhood. They are characterized by their poor prognosis. Vaginal location is very rare after puberty and exceptional in the post menopause. Treatment is based on several therapeutic measures combining neoadjuvant chemotherapy followed by surgery and/or external beam radiation therapy. We report herein the case of a 25 years-old woman, presented with vaginal embryonal RMS revealed by metrorrhagia and pelvic pain. The diagnosis was confirmed by biopsy and histopathological study. Pre-treatment workup was negative for metastatic disease. She has received chemotherapy based on vincristine, doxorubicin, and cyclophosphamide. The clinical evolution was marked by improvement of symptoms, unfortunately the patient died following febrile neutropenia after the third cycle of chemotherapy.
Rhabdomyosarcoma (RMS) is the most common soft tissue tumor in children, representing approximately 50% of all soft tissue sarcomas and 3% to 4% of all cancers [1]. The genitourinary tract is the second most common primary site after the head and neck region [2]. Embryonal RMS is the most common type (60-70% of all RMSs) arising in the pediatric female genitourinary tract [3], it occurs frequently in the vagina (median age 1.8 years). In contrast, uterine RMSs were most often seen during adolescence up to 20 years of age. Vaginal embryonal RMS is rare after puberty and exceptional in postmenopausal woman, accounting for 3% of all soft tissue sarcoma in adult woman [1,4]. Treatment is mainly based on chemotherapy followed by surgery and/or radiation therapy, but the prognosis of these lesions remains poor in adults. We report the case of a primary RMS of the vagina in 25 years-old woman, while discussing epidemiology, diagnosis, and treatment of this rare entity.
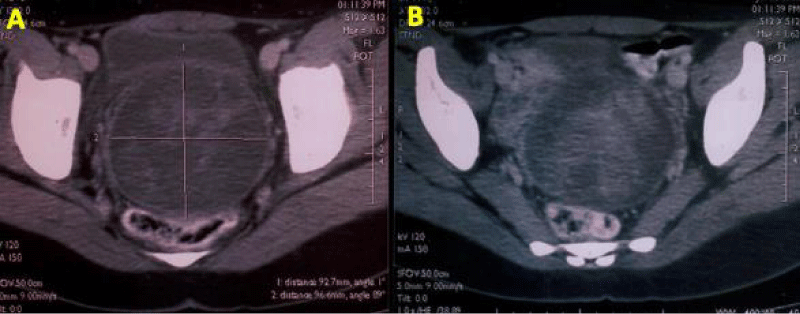
A 20 years-old Arabic woman, with no significant past medical history, presented to our department with complaints of metrorrhagia and pelvic pain 9 months before. Physical exam found a pelvic mass. The gynecological examination, showed a giant mass protruding from the vagina with bilateral extension to the parametrium on rectal examination. There was no inguinal, axillary or supraclavicular adenopathy. Pelvic ultrasound revealed a hypoechoic and heterogeneous vaginal mass with extension to the cervix and lower third of uterus, measuring 12x9x7cm in diameter. A computed tomography (CT) scan of the pelvis showed a bulky vaginal and cervical mass measuring 13 x 8 cm in maximal diameter, with extension to the lower third of the uterus and internal two thirds of parametrium (Figure 1A,B). A punch biopsy with histological examination confirmed the diagnosis of embryonal rhabdomyosarcoma. Workup including CT scan of the thorax and abdomen was negative for metastatic disease. The patient has received chemotherapy containing vincristine, doxorubicin, and cyclophosphamide (VAC). Clinical evaluation after the third cycle was marked by pain relief and regression of tumor volume. Unfortunately, the patient presented a febrile neutropenia leading to her death.
Figure 1: (A, B): axial CT scan of the pelvis showing a giant vaginal mass with extension to the cervix and lower third of uterus.
Epidemiology
RMS of the female genital tract most often arise in the vagina with about 90% of the cases occurring in children under 5 years of age [1], but it may also affect the uterine cervix [4]. It’s very rare for vaginal RMSs to occur in patients over 20 years of age [1], as in our case. The majority of RMSs cases appear sporadically with no recognized predisposing factor or risk factors, although a small proportion is associated with some genetic conditions [5].
Diagnosis and workup
Clinically, the most common symptoms are: feeling of a mass in the introitus, vaginal bleeding and pelvic pain. Additional symptoms included leucorrhea and malodorous discharge [6]. It appears also as benign polyp which may cause delay in diagnosis [7]. Imaging plays a crucial role not only in the initial diagnosis but also in long term follow-up of genital RMSs. Ultrasonography is often the first imaging modality for soft tissue masses. As in the present case on US, RMS presents as lightly hypoechoic heterogenous mass. It can also reveal pelvic retroperitoneal lymphadenopathy [3]. MRI which is the gold standard imaging modality in RMS shows low to intermediate signal intensity on T1‑weighted images and on T2‑weighted images they tend to be of intermediate‑to‑high signal intensity [3].
Histopathology
Botryoid aspect which means a “bunch of grapes”, characteristically describes the clinical appearance of the tumor. This macroscopic variant is due to its growth pattern (primary exophytic and non-invasive) [8]. Microscopically we find rhabdomyoblasts, and small round to oval spindled cells [9]. Pathologic differential diagnosis includes benign entities such as rhabdomyoma and an edematous mesodermal cervical polyp (pseudosarcoma botryoides), and malignant entities such as adenosarcoma and other “small, round, blue cell” tumors [10,11].
Treatment and prognosis
Treatment of adult RMS of lower genital tract is necessarily multimodal, in all cases combining chemotherapy with locoregional treatments, essentially surgery and/or radiotherapy. But unlike children’s RMSs, there are no consensus guidelines, nor standardization of therapeutic sequences. RMS is intrinsically sensitive to chemotherapy, it must therefore be an integral part of the therapeutic strategy, with a double objective: on the one hand it can significantly reduce the tumor size and thus facilitate locoregional treatment and enhance local control, with increasingly conservative approaches, on the other hand chemotherapy will eradicate micro metastatic systemic disease, most likely already existing at the time of initial diagnosis [9]. VAC is the most used regimen, with objective responses of up to 80%. The current paradigm of surgical treatment of RMSs is complete wide excision of the primary tumor with a margin of uninvolved tissue whenever possible. Debulking and mutilating procedures should be avoided [9]. As for surgical treatment, according to the extent of tumor and the age of the patient, the surgical procedures vary from local excision, polypectomy, and partial or complete vaginectomy to radical hysterectomy [1]. It is performed to establish definitive diagnosis, to reduce tumor burden, to minimize the symptomatology of vaginal discomfort and bleeding [12]. It may also preserve function of vagina, uterus and ovaries if possible or necessary, especially when the patient is in reproductive age [1]. Another therapeutic option has been described in management of embryonal RMS of genital tract is radiotherapy, it is reserved for patients with residual macroscopic or suspected microscopic disease after resection, or for salvage therapy in the recurrent setting for patients of advanced age who could not tolerate intensive chemotherapy [6,13]. Compared to children’s RMS, the prognosis is poor and therefore treatment should be started as soon as possible to give the maximum chance of remission. The presence of distant metastasis at the diagnosis, quality of surgery and poor response to preoperative chemotherapy are strongly associated with poor prognosis (Table 1).
| Table 1: publications of adult female genital tract rhabdomyosarcomas. | ||||
| Author | Number of cases | Histology | Tumoral site | Treatment |
| Baiocchi, et al. [2] | 1 | Embryonal RMS | Cervix | Radical hysterectomy + chemotherapy |
| Ditto, et al. [4] | 1 | Botryoid ERMS | Cervix | Surgery+ chemotherapy+ radiotherapy |
| Behtash, et al. [5] | 2 | Botryoid ERMS | Cervix | Surgery + chemotherapy |
| Dehner, et al. [6] | 14 | Embryonal RMS | Cervix | Conservative surgery + chemotherapy |
| Saadi, et al. [8] | 1 | Botryoid ERMS | Cervix | Chemotherapy + surgery |
| Sanders, et al. [10] | 1 | Embryonal RMS | Cervix | Radical hysterectomy + chemotherapy |
| Kriesman, et al. [14] | 11 | Embryonal RMS Botryoid (8 cases) |
Cervix | Surgery+ chemotherapy+ radiotherapy |
| Ojwang, et al. [15] | 1 | Embryonal RMS | Uterus | Chemotherapy + surgery |
| Kim, et al. [16] | 1 | Spindle cell RMS | Uterus | Surgery |
| Hemida, et al. [17] | 10 | Embryonal RMS | Vagina Cervix |
Biopsy only Surgery + chemotherapy + radiotherapy |
| Kirsch, et al. [18] | 67 | Embryonal RMS (85%) | Female genital tract | Surgery+ chemotherapy+ radiotherapy |
| Fukunaga, [19] | 1 | Alveolar RMS | Uterine corpus | Surgery + chemotherapy |
| Chmaj‐ Wierzchowska, et al. [20] | 1 | Pleomorphic RMS | Uterine corpus | Surgery + chemotherapy |
| Adams, et al. [21] | 1 | Embryonal RMS | Cervix | Chemotherapy + surgery |
| Nasioudis, et al. [22] | 144 | Embryonal (75.7%) | Vagina :51.4 % Vulva and the cervix :48.6 % | Surgery Primary radiotherapy Chemotherapy Multimodal |
Embryonal RMS is the most common malignancy arising in the pediatric female genitourinary tract. Vaginal location is rare in adult. Its management requires multidisciplinary combination of several therapeutic modalities to improve prognosis. Primary chemotherapy using VAC regimen is the preferred approach.
Data sharing: not applicable to this article as no datasets were generated or analysed during the current study
Consent
“Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.”
Authors’ contributions
All authors read and approved the final manuscript.
- Ries LAGHD, Krapcho M, Mariotto A, Miller BA, Feuer EJ, et al. SEER Cancer Statistics Review, 1975–2003. Bethesda: National Cancer Institute; 2006.
- Baiocchi G, Faloppa CC, de Toledo Osorio CA, Kumagai LY, Fukazawa EM, et al. Embryonal rhabdomyosarcoma of the uterine cervix in a 47-year-old woman. J Obstet Gynaecol Res. 2011; 37: 940–946.
- Chauhan RS, Singh DK, Guha B, Kumar> I, Verma A. Multimodality imaging of vaginal rhabdomyosarcoma Genitourinary .Indian J Radiol Imaging. 2017; 27: 148–151. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5510311/
- Ditto A, Martinelli F, Carcangiu M, Solima E, de Carrillo KJA, et al. Embryonal rhabdomyosarcoma of the uterine cervix in adults: a case report and literature review. J Low Genit Tract Dis. 2013; 17: e12‐e17. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23903199
- Behtash N, Mousavi A, Tehranian A, Khanafshar N, Hanjani P. Embryonal rhabdomyosarcoma of the uterine cervix: Case report and review of the literature. Gynecologic Oncology. 2003; 91: 452-455. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14599884
- Dehner LP, Jarzembowski JA, Hill DA. Embryonal rhabdomyosarcoma of the uterine cervix: a report of 14 cases and a discussion of its unusual clinicopathological associations. Mod Pathol. 2012; 25: 602–614. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22157934
- Kriseman ML, Wang WL, Sullinger J, Schmeler KM, Ramirez PT, et al. Rhabdomyosarcoma of the cervix in adult women and younger patients. Gynecol Oncol. 2012; 126: 351–356. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939703/
- Saâdi I, Errihani H, Haddadi K, Amaoui B, Benjaafar B, et al. Rhabdomyosarcome botryoïde du col utérin: à propos d’un cas Sarcoma botryoïde of the uterine cervix. Canc/Radiother. 2002; 6: 363–365.
- Van Rijn R, Wilde JCH, Bras J, Oldenburger F, McHugh K, et al. Imaging findings in noncraniofacial childhood rhabdomyosarcoma. Pediatr Radiol. 2008; 38: 617‑634. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18324394
- Sanders MA, Gordinier M, Talwalkar SS, Moore GD. Embryonal rhabdomyosarcoma of the uterine cervix in a 41-year-old woman treated with radical hysterectomy and adjuvant chemotherapy. Gynecol Oncol. 2008; 111: 561–563. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4092352/
- Fletcher C, Bridge J, Hogendroom P, Mertrens F. WHO Classification of Tumours of Soft Tissue and Bone. Lyon: IARC; 2013.
- Andrassy RJ, Wiener ES, Raney RB, Hays DM, Arndt CA, et al. Progress in the Surgical Management of Vaginal Rhabdomyosarcoma: A 25-year Review From the Intergroup Rhabdomyosarcoma Study Group. J Pediatr Surg. 1999; 34: 731-734. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10359173
- Copeland LJ, Sneige N, Stringer CA, Gershenson DM, Saul PB, et al. Alveolar rhabdomyosarcoma of the female genitalia. Cancer. 1985; 56: 849-855. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/4016676
- Kriseman ML, Wang WL, Sullinger J, et al. Rhabdomyosarcoma of the cervix in adult women and younger patients. Gynecol Oncol. 2012; 126: 351‐356. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939703/
- Ojwang SB, Rana F, Sayed S, Aruasa WK. Embryonal rhabdomyosarcoma with uterine inversion: Case report. East Afr Med J. 2006; 83: 110‐113. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16771108
- Kim DW, Shin JH, Lee HJ, Hong YO, Joo JE, et al. Spindle cell rhabdomyosacoma of uterus: A case study. Korean J Pathol. 2013; 47: 388‐391. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3759640/
- Hemida R, Goda H, Abdel‐Hady el‐S, El‐Ashry R. Embryonal rhabdomyosarcoma of the female genital tract: 5 years’ experience. J Exp Ther Oncol. 2012; 10: 135‐137. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23350353
- Kirsch CH, Goodman M, Esiashvili N. Outcome of female pediatric patients diagnosed with genital tract rhabdomyosarcoma based on analysis of cases registered in SEER database between 1973 and 2006. Am J Clin Oncol. 2014; 37: 47‐50. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23111355
- Fukunaga M. Pure alveolar rhabdomyosarcoma of the uterine corpus. Pathol Int. 2011; 61: 377‐381. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21615615
- Chmaj‐Wierzchowska K, Wierzchowski M, Szymanowski K, Czerniak T, Mróz M, et al. Pleomorphic rhabdomyosarcoma of the uterine corpus ‐ A case report. Ginekol Pol. 2010; 81: 541‐543. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20825058
- Adams BN, Brandt JS, Loukeris K, Holcomb K. Embryonal rhabdomyosarcoma of the cervix and appendiceal carcinoid tumor. Obstet Gynecol. 2011; 117: 482‐484. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21252797
- Nasioudis D, Alevizakos M, Chapman-Davis E, Witkin SS, Holcomb K. Rhabdomyosarcoma of the lower female genital tract: an analysis of 144 cases. Arch Gynecol Obstet. 2017; 296: 327‐334. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28634755