More Information
Submitted: August 06, 2022 | Approved: September 01, 2022 | Published: September 03, 2022
How to cite this article: Suresh K. Prostate health in India (BPH &Prostate Cancer). Arch Cancer Sci Ther. 2022; 6: 009-017.
DOI: 10.29328/journal.acst.1001028
Copyright License: © 2022 Suresh K. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Prostate gland; Benign Prostate Hyperplasia (BPH); Cancer of Prostate (CAP); Cancer registries; Ultrasound (KUB); Prostate-Specific Antigen (PSA); Alpha-blockers; 5 alpha-reductase inhibitors & Transurethral Resection of the Prostate (TURP); Chemotherapy and Hormonal therapy
Prostate health in India (BPH & Prostate Cancer)
Suresh Kishanrao*
MD, DIH, DF, FIAP, FIPHA, FISCD, Public Health Consultant, Bengaluru, India
*Address for Correspondence: Suresh Kishanrao, MD, DIH, DF, FIAP, FIPHA, FISCD, Public Health Consultant, Bengaluru, India, Email: [email protected]
The prostate gland, found only in men, is an extremely important organ of the reproductive system, but it is not taken care of adequately, leading to prostate inflammation and benign hypertrophy or even cancer. Benign prostate enlargement compresses urine flow through the urethra, leading to uncomfortable urinary symptoms. Hyperplasia increases the risk of bladder stones, urinary tract infections, and kidney problems. In India prevalence of Benign Prostrate Hyperplasia (BPH) is around 50% of men by the age of 60 years. Studies suggest that benign prostatic hyperplasia is a result of the disproportion between oestrogen & testosterone. A higher proportion of oestrogen within the prostate boosts the growth of prostate cells. The management of BPH is streamlined in recent times and the majority are on medical treatment.
Prostate cancers are one of the cancers showing a significant increase in incidence along with mouth and kidney and lung cancers among the male population. With an estimated population of 1400 million and about 98 million males over 50 years of age in mid-2022 and the average life expectancy increasing 68.4 years, has a bearing on the changing incidence and pattern of prostate cancer in the current decade in India. Based on the five population-based cancer registries in 2009-10, the age-adjusted annual incidence rates per lakh population of prostate cancers were highest in Delhi (10.2) followed by Bengaluru (8.7), Mumbai (7.3), Chennai (7) and Bhopal (6.1). Cancer can co-exist with BPH. Prostate cancer management is still in the development stage with a 5-year life expectancy of around 64%.
The prostate is the second leading site of cancer among males in large Indian cities like Delhi, Kolkata, Pune, and Thiruvananthapuram, and the third leading site of cancer in cities like Bangalore and Mumbai. Despite the limitations of diagnosis, the annual cancer incidence rate ranges from 5.0-9.1 per 100,000/year, as compared to the rates in the United States and other developed countries of 110 &180 for whites and blacks respectively.
This article is a review of Prostate health in India based on a personal observation of around 183 cases by the author in the last 10 years.
Materials & methods: This is an observational study report of three cohorts of men across the country. The sample was of people encountering the author. The sample included i) 69 septuagenarians plus ii) 30 senior citizens aged 60 - 70 years and iii) 84 men in 40 – 60 - year age groups over the last decade. The data source was sharing annual check-up reports or consultation report in person for seeking 2nd opinion. A minimum of 2 consultations, first when diagnosed and the recent between July 2021 to June 2022.
The prostate, or the frontal gland, found only in men is an extremely important organ for the male reproductive system. This walnut-sized gland is located under the bladder. It secretes prostatic fluid, the main component of semen. Hyperplasia of the prostate most commonly involves the transitional zone (periurethral zone), affecting both the glandular and stromal tissue. Although very important in male organs, being invisible, it is not taken care of adequately leading to most men suffering from prostate inflammation and even cancer. Men under the age of 45 have an enlarged prostate and are asymptomatic. After 45 years about 80% suffer from Enlarged Prostate in their lifetime.
Benign prostatic hyperplasia (BPH), also known as senile enlargement of the prostate (SEP), adenoma, adenomyoma, and nodular hyperplasia of the prostate (NHP) refers to an enlargement of the prostate gland, the most common disease in elderly men, especially those aged above 50 years. In India, multiple studies have indicated the prevalence of Benign Prostrate Hyperplasia (BPH) to be around 25%, 37%, 37% and 50% for the age group 40 – 49, 50 – 59, 60 – 69 and 70 – 79 years, respectively. By the age of 60 years, more than 50% of men would have some evidence of the disease. Worldwide, the prevalence of BPH generally varies from 20% to 62% in men beyond the age of 50 years [1].
Clinical BPH is defined as having at least two of the following features: (A) Moderate to severe lower urinary tract symptoms (LUTS) with International Prostate Symptom Score (IPSS) greater than 8 and (B) an enlarged prostatic volume > 30 mL) and (C) maximum urinary flow rate less than 15 mL/s [2].
Benign prostatic hyperplasia cause symptoms that affect urine flow, like decreased or weak flow of urine, nocturia, the sensation of incomplete bladder emptying, multiple interruptions in urination, difficulty in starting urination, or need to strain to pass urine, dribbling at the end of urine flow, frequent urge, and urgency to urinate, pain while urinating or ejaculation. If neglected complications like development of bladder stone, bladder infection, damage to kidneys because of backpressure, blood, or pus in the urine, experiencing pain in the lower part of the abdomen or genitals during urination, inability to urinate, chills or fever while urinating may occur. In severe cases, kidney damage and the development of chronic kidney disease and renal failure are also observed. Among the side effects, erectile dysfunction, loss of libido, and ejaculatory disorder may be nagging the person, impacting the individual’s mental health.
Risk Factors for Benign Prostatic Hyperplasia include- age 40 years or above, a family history of BPH, associated medical conditions such as cardiovascular problems, obesity, type 2 diabetes, lack of physical exercise, and a sedentary lifestyle. They will have erectile dysfunction.
The second problem for men due to the prostate is Cancer of the Prostate (CAP). Prostate cancer is primarily a disease of elderly men over 65 years of age. It is opined that prostate cancer is the second most frequently diagnosed cancer and the sixth leading cause of cancer deaths in men worldwide and the fifth most common cancer overall. It is estimated cost 4.04 million years of healthy life are lost globally due to prostate cancer alone [3]. Data regarding the true incidence of prostate cancer in India is limited.
Prostate cancers are one of the cancers showing a significant increase in incidence along with mouth and kidney and lung cancers among the male population globally. An estimated population of 1400 million and about 98 million males over 50 years of age in mid-2022 and the average life expectancy increasing to 68.4 years, that has a bearing on the changing incidence and pattern of prostate cancer in the current decade in India. Based on the five population-based cancer registries in 2009-10, the age-adjusted annual incidence rates per lakh population of prostate cancers were highest in Delhi (10.2) followed by Bengaluru (8.7), Mumbai (7.3), Chennai (7) and Bhopal (6.1). Cancer can co-exist with BPH. Cancer management is still in the development stage with a 5-year life expectancy of around 64% [4].
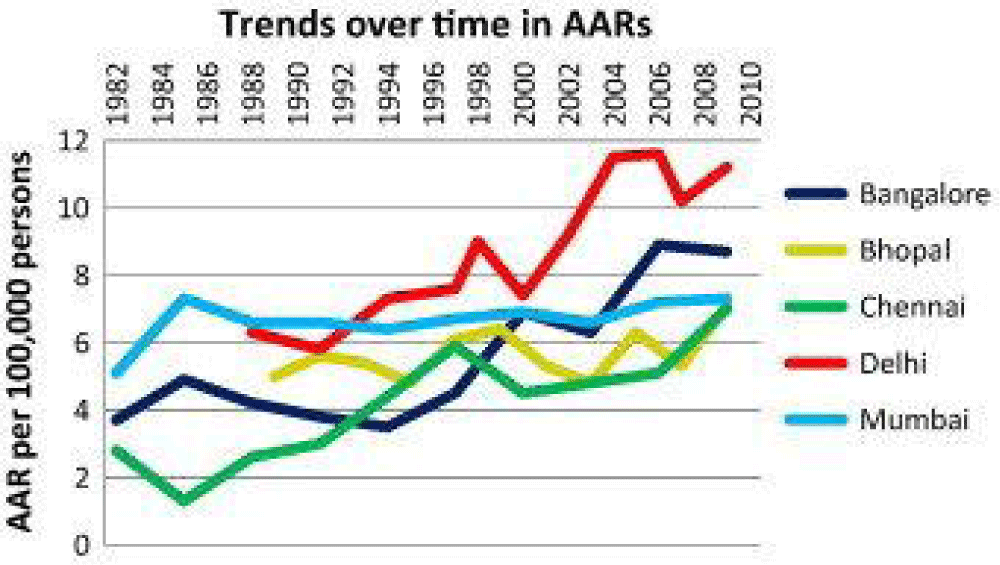
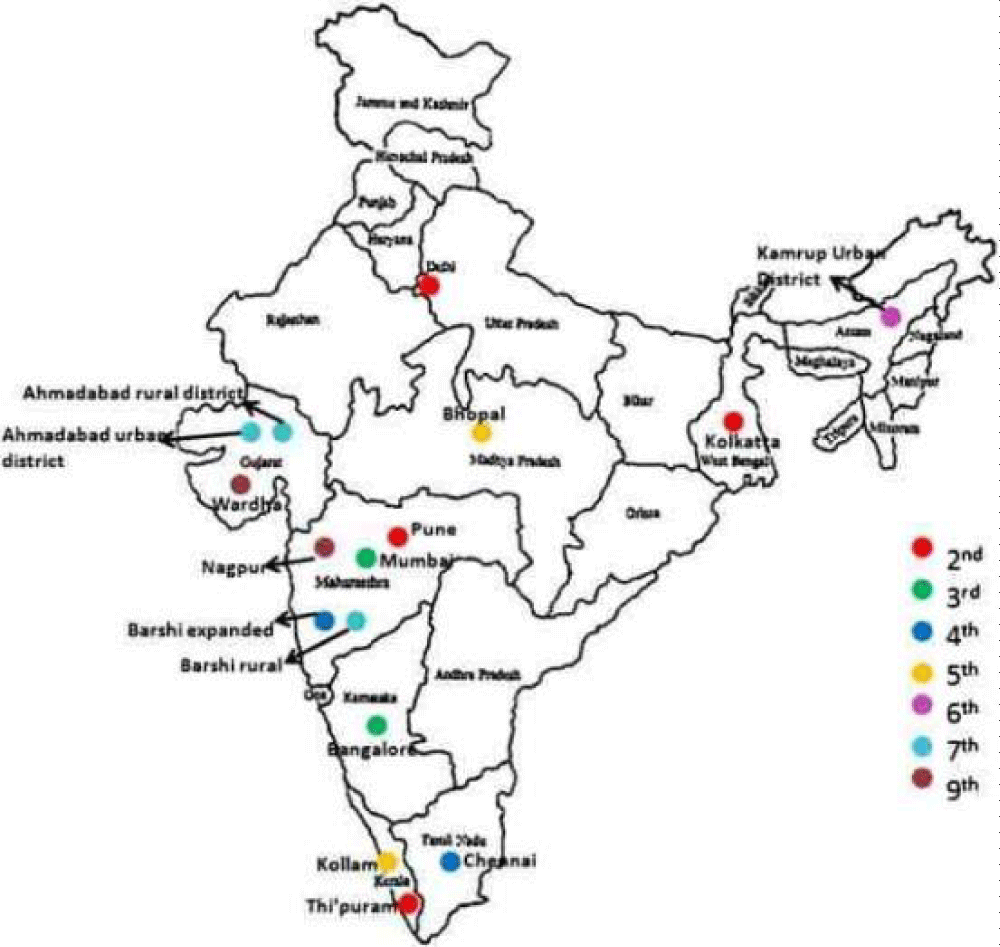
The table, map and graphs summarise the organs getting affected, Trends of CAP, diagnostic exams, and treatment available in India as of now Table 1, Figures 1,2.
| Table 1: Organ involved, differential diagnosis, diagnostic tools, and treatment available in India-2022. | |||
| Organs Involved | Differential Diagnosis | Examinations | Treatment |
| Prostate gland | Prostate Cancer | Digital Rectal exam | Alpha-blockers: Prazosin, Terazosin, Tamsulosin |
| Bladder | Bladder stones | Ultrasound KUB | Tadalafil |
| Kidney | Bladder trauma | Intravenous (IVP) Pyelogram | 5 alpha-reductase inhibitors: Finasteride, Dutasteride |
| Overreactive bladder | Cystoscopy | Transurethral resection of the prostate (TURP) | |
| Uroflowmetry | Transurethral incision of the prostate (TUIP) | ||
| Prostate-specific Antigen (PSA) test | Transurethral microwave thermotherapy, Ablative laser therapy, Enucleation procedure & Prostatic urethral lift | ||
Figure 1: Trends of Prostate Cancers in India.
Figure 2: A map of India showing the rank of prostate cancer among the top ten leading sites of all cancers, for different population-based cancer registries of India.
The basis of this article is the observation of about 69 septuagenarians + -, my age cohorts, another 30 senior citizens aged less than 70 years, and 84 men in 40–60-year age groups over the last decade. The methodology included sharing of annual check-ups; consultation report (verbal/documents) is personal discussions seeking 2nd opinion. A minimum of 2 consultations first when diagnosed and the recent between July 2021 to June 2022.
We lost one of our close friends, a well-known 75 yrs. plastic surgeon for CAP in mid-2021.
The distribution of study subjects is as given Tables 2-4.
| Table 2: Summary of the observed in our patients. | ||||
| Age group & No ofClients | Clients’ time ofacquaintance | Type of ContactsReviewed | Conditions &Numbers | Type of Management |
| 50- 59 (57) | 5- 15 Years | 2ndopinion Consultations - 57 | BPH6 | BHPMT-6 |
| 60- 69 (30) |
5- 10 years | Relatives& Apt. colleagues -13 | BHP-8 | BHPMT-8- BHPST-1 |
| >10 years | WorkplaceColleagues -17 | BHP-9 | BHP-MT-8,BHPST-1 | |
| 70- 79 | <10 Years | Relatives& Apt. colleagues -11 | BHP-7,& CAP-1 | BHPMT-7,CAP+ S & Ch |
| 10- 20 Years | WorkplaceColleagues -11 | BHP-8,CAP-1 | BHPMT-6,BHPST-2, CAP-S& ImmunoT | |
| >20 years | 1968MBBS classmates - 28 | BPH-14,CAP-2 | BHPM-9,BHPST-5, CAP-1 S, 1-CH +H | |
| 80+ | MedicalCollege Seniors - 5 | BHP-3,CAP-1 | BHPM-2,BHPST-1, CAPS 1 S & Chemo | |
| Residentialcomplex Sr-10 | BHP-7,CAP-1 | BHPM-5,BHPST-2, CAP = S+ Immuno T | ||
| Others-4 | BHP-3,CAP-1 | BHPM-3,CAP-ST | ||
| Total | 183 | BHP-68, CAP-7 Normal-108 |
BHMT-54, BHPST = 12 CAP= S = 2, S+ Chemo = 2 & S+CH+Immuno T = 3 |
|
| Note:BPH: Benign Prostate Hypertrophy; CAP: CancerProstate; BHPMT: Medical Therapy for BHP; ST: Surgical Treatment (TURP/TUIP);Chemo: Chemotherapy; Immuno T: Immunotherapy | ||||
| Table 3: Common Symptom in BHH Cases. | ||
| Sl. No | Symptoms | Frequencies (n = 68) |
| 1 | Nocturia | 50 (74%) |
| 2 | Urgency to urinate | 35 (51%) |
| 3 | Dribbling of urine | 28 (41%) |
| 4 | Interrupted urination | 23 (34%) |
| 5 | Needed to strain to pass urine | 20 (29%) |
| 6 | Incomplete bladder evacuation sensation | 12 (18%) |
| Table 4: Common Symptoms among Cancer clients. | ||
| Sl. No | Symptoms | Frequencies (n = 7) |
| 1 | Nocturia | 6 |
| 2 | Painful micturition | 5 |
| 3 | Blood in urine | 4 |
| 4 | Dribbling of urine | 3 |
The prostate gland is controlled by powerful sex hormones, including testosterone. In the prostate gland, testosterone is converted to another hormone called dihydrotestosterone (DHT). High levels of DHT cause the cells in the prostate to enlarge. The prostate is designed by nature to produce the highest quality sperm, to produce life as healthy and strong as possible. Xenoestrogens, synthetic or body-produced compounds of the female hormone oestrogen, are one of the most common toxins found in the human body today. In men, the prostate takes care of removing these hormonal compounds. Xenoestrogens disrupt the normal balance of oestrogen and testosterone, which promotes prostate enlargement. Oxidative stress, one of the main causes of any degenerative disease, inevitably affects the prostate. Certain foods and beverages are known to have an impact on prostate health because of their effects on testosterone and other hormones.
Current research points to the fact that a diet primarily consisting of meat or dairy products can increase the risk of prostate enlargement and cancer, especially among people who do not incorporate enough vegetables into their diet.
An enlarged prostate is common in men over 50 years, as the prostate gets bigger as an individual gets older. It is not cancer and there are simple ways to treat it. BPH can co-exist with CA Prostate. An enlarged prostate gland can cause uncomfortable urinary symptoms, such as blocking the flow of urine out of the bladder, and 2. Prostatitis – a kind of urinary tract infection in men if neglected may lead to kidney failure.
If the cells grow in an un-uncontrolled manner inside the prostate, that leads to cancer. Prostate cancer is the most common and accounts for nearly one-third of all male cancers. The majority of men diagnosed with prostate cancer are older, it can affect younger men, too. In the Western world, 40% of this Cancer occurs in men < 65 years of age. In our observation, all 7 CAP cases were among men over 70 years. Though not everyone with a family history of prostate cancer will get it, a positive family history will double the risk as compared to the general population. I was not able to track the family history of CAP in more than 1 case for want of genetic testing. Proper screening can easily detect and treat prostate cancer if done in earlier stages.
Prostate cancer is one of the top ten leading cancer in India. Recently there has been an increase in reports of cancer in younger men in the age group of 35 - 44 and 55 - 64 residing in metropolitan cities. Old age, obesity, improper diet, and genetic alterations have been identified as some of the main contributing factors to an increased cause of prostate cancer. The incidence rates of this cancer are constantly and rapidly increasing, and the projection data shows that the number of cases would have doubled to over 56,000 by the end of 2021. (Prostate Cancer Is the Leading Cancer in India, https://cytecare.com/blog/).
Currently, serum PSA is used by most family doctors as a screening tool for prostate cancer normal PSA does not rule out prostate cancer, as roughly 25% of prostate cancers have normal PSA. The rise in serum PSA can occur in a variety of conditions ranging from a simple physical examination to prostate infection and surgery to prostate cancer. A rising level should be the trigger to look for prostate cancer but it’s usually due to benign enlargement of the gland. One of the common misperceptions is that prostate problems always necessitate surgery; however, the fact is, many times, prostate problems can be treated with medications. In this observational study also (55/68) 80% of cases are being managed by medical therapy.
The projected cancer burden in India for 2021 was 26.7 million DALYs AMI and is expected to increase to 29.8 million by 2025. The highest burden was in the north (2408 DALYs AMI per 100,000) and north-eastern (2177 DALYs AMI per 100,000) regions of the country and higher among males. More than 40% of the total cancer burden was contributed by the seven leading cancer sites — lung (10.6%), breast (10.5%), esophagus (5.8%), mouth (5.7%), stomach (5.2%), liver (4.6%), and cervix uteri (4.3%) and Prostate (4%) [10].
The Contribution of DALYs from cancer by different sites, sex and overall (Percentage), Prostate cancer was at number 11 among all cancer in men contributing to 3.15 of all cancers.
The management of prostate cancer is multidisciplinary and often involves minimally invasive surgery like robotic or Laparoscopic surgery and/or Radiation therapy. Advanced cases may need various types of chemotherapy and immunotherapy etc. Among our 7 cases 3 needed combination surgery, chemotherapy, and immunotherapy, while 2 had surgery followed by chemotherapy. Only 2 had CURT. As radical surgical treatment may lead to minor incontinence/impotence; currently Laparoscopic and Robotic surgery is used followed by radiation or chemotherapy or immunotherapy.
A study in the USA, using the National Cancer Database, looked at a data set of 24,679 patients diagnosed with T1a/b prostate cancer between 2010 and 2017 and inferred that T1a/b prostate cancer represented 3.5% of all prostate cancer without a change in incidence over time. It suggested that T1a/b prostate cancer significantly increased from 38.8% in 2010 to 44.1% in 2017 (p < .001). The chance of being diagnosed with T1a/b non-clinically significant disease decreased from 61.3% in 2010 to 55.9% in 2017. Patients diagnosed with T1a/b disease were significantly older (mean age 72.2 ± 9.6 vs. 64.2 ± 8.1; p < .001) than patients diagnosed with T1c disease. Patients with T1a/b disease were less likely to be treated definitively with surgery or radiation compared with patients with T1c disease [11].
Family doctors should always advise their patients to have a routine check-up for their prostate health and awareness and get it cured if there are any problems.
1. The diagnostic tool available for prostatic health are digital rectal exam: A gloved hand inserted through the anus into the rectum can feel the prostate’s shape, thickness, and size.
2. Prostate-Specific Antigen (PSA) test: Prostate-specific antigen is a compound released by the prostate. In an enlarged prostate, the levels of PSA will increase. It helps detect 70% - 75% of prostate cancers, as PSA levels can be elevated due to recent procedures, surgeries, or infections also.
3. Cystoscopy: A hollow tube called a cystoscope fitted with a lens is inserted inside the urethra and slowly advance the cystoscope inside your bladder and visualize the bladder.
4. Ultrasound: Ultrasound of the kidneys and urinary bladder (USG KUB) has become the standard first-line investigation after the urologist’s finger, to evaluate the size and volume of the prostate gland.
5. Intravenous Pyelogram (IVP): An intravenous pyelogram (IVP) is a type of x-ray that provides images of the urinary tract. After injecting a contrast dye into one of your veins. The dye travels through your bloodstream and into your urinary tract and helps in the detection of an enlarged prostate. IVP is not commonly used these days.
6. Urine tests: A urine test helps to rule out any infection /urinary conditions that cause similar symptoms.
7. Urinary flow test: This test measures the strength and amount of urine flow, urinated into a receptacle that is attached to a machine. It helps in monitoring prognosis over time after initiating therapy.
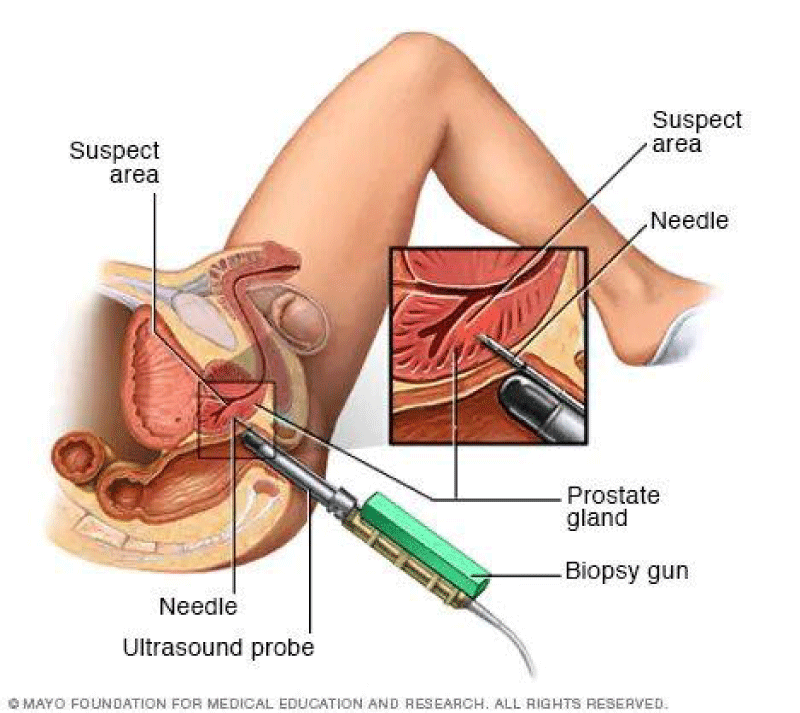
8. Postvoid residual volume test: This test evaluates if a patient can fully empty your bladder while urinating, through ultrasound, or by inserting a catheter into your bladder after you finish urinating Figure 3.
Figure 3: Transrectal Prostate Biopsy.
9. 24-hour voiding diary: You will be asked to maintain a record of the frequency and amount of urine to see if more than one-third of your daily urine output occurs during the night.
10. Prostate biopsy: A prostate biopsy uses a needle guided inside the rectum to take tissue samples of the prostate. Examining the tissue microscopically will histopathologists identify if cancer cells are seen in the tissue or not. For a prostate biopsy, tissue samples can be collected in two ways:
1. Transrectal biopsy: This is the most common method of performing a prostate biopsy. In this, the biopsy needle is passed through the wall of the rectum to collect the samples.
2. Transperineal biopsy: This procedure requires an MRI or CT scan. The biopsy needle is inserted through a small cut made on the perineum (the area of skin) between the anus and scrotum, and samples of the tissue are collected.
11. Urodynamic and pressure flow studies: This test allows doctors to measure and determine how well your bladder muscles are functioning. A catheter is inserted inside your urethra and into your bladder. Water or air is slowly injected into the bladder, which allows for the evaluation of muscle functioning [6].
Diagnostics
Before 1980, patients having BPH were evaluated only with the medical history and digital rectal examination and urinalysis, using a few blood investigations and radiography to rule out any damage to the urinary tract or differential diagnosis.
After 1980, i) Ultrasonography, computed tomography, and urodynamic measures enable the accurate measurement of post-void residual urine along with the size of the prostate gland. ii) Measuring serum prostate-specific antigen (PSA) has also become a routine procedure in male patients with urine voiding problems.
American Urological Association Symptom Index (AUA-SI) or IPSS is the most reliable scale for monitoring BPH patients, the severity of the disease, and for planning the management of the disease. The management guided by this involves i) when the symptoms are mild (IPSS < 8), watchful waiting is to be followed, ii) when the symptoms are moderate to severe (IPSS ≥ 8), the treatment plan must be devised and iii) in case of complications, surgical intervention is obligatory. Invasive techniques like pressure flow studies or formal urodynamic studies are good to determine the obstruction at the neck of the urinary bladder, but these are optional tests and are needed in case the symptoms are severe or surgical intervention is chosen for the management.
Prostate cancer is diagnosed with patient history and physical examination, including a digital rectal examination to feel the size, texture, and firmness of the prostate, lumps, hard areas, or growths beyond the prostate, and pain when touching or pressing the prostate.
Other tests to diagnose prostate cancer- Blood tests to check prostate-specific antigen (PSA) levels, Prostate health index (PHI) blood test, Prostate cancer urine test, and Imaging like Magnetic resonance imaging (MRI) and Transrectal ultrasound (TRUS) and prostate biopsy.
Of late MRI-targeted biopsies with a new prostate cancer risk score have cut the number of unnecessary biopsies in half while still detecting clinically significant cancers. {European Association of Urology 2021 Annual Meeting (EAU 2021)}. A trial of nearly 2300 men with elevated prostate-specific antigen (PSA) levels and/or high scores on the Stockholm 3 predictive test, were randomly assigned to undergo either systematic biopsy or Stockholm 3 testing plus MRI with biopsy only of suspicious lesions. The results show that the MRI-targeted strategy was associated with a 52% reduction in biopsy procedures compared with the systematic approach and a 69% reduction in the detection of low-grade (Gleason score 6) cancers, as reported by the Karolinska Institute, in Stockholm, Sweden.
“Combining the Stockholm 3 test with an MRI-targeted biopsy approach for prostate cancer screening decreases over detection, maintaining better detection of prostate cancer.
The Stockholm 3 test
Developed at the Karolinska Institute, includes clinical variables (age and previous biopsy status) and a single-nucleotide-based genetic score, as well as measurements of five protein levels: total PSA, free PSA, human kallikrein 2, microseminoprotein-beta, and macrophage inhibitory cytokine 1.
MRI-Guided Biopsy Studies: Several recent major clinical trials have highlighted the advantages and potential drawbacks of MRI-targeted biopsy compared with transrectal ultrasound-guided 12-core systematic biopsy. The MRI-guided technique identified more clinically significant cancers and reduced the need for biopsy.
Back home, Thakur, et al. have suggested the utility of the f/t PSA ratio in the diagnosis of prostate cancer [7] and Malati, et al. studied PSA levels in the Indian population in 2006 in 583 healthy males, 1,090 patients with BPH, and 651 patients with adenocarcinoma prostate in Andhra Pradesh in South India. They found that the PSA level was significantly high in BPH patients and adenocarcinoma prostate patients, compared to healthy males [8].
Currently, in India, the most common investigation done for all prostate enlargement/cancer cases is PSA assessment in urine, followed by Pelvic scanning or X-ray or MRI (50%) and biopsy in Cancer suspected cases. In our study, these tests were done in most cases.
Pathophysiology
Men produce testosterone, the primary male sex hormone, throughout their lives, along with a minute amount of oestrogen. With declining age, the testosterone produced by the body reduces resulting in an increased proportion of oestrogen in the system. Studies suggest that benign prostatic hyperplasia results due to this disproportion between oestrogen and testosterone. The high level of oestrogen within the prostate boosts the activity of substances that increase the growth of prostate cells.
Management
In my prime professional life before 1990, prostatectomy was considered the only accepted treatment for BPH. Transurethral incision of the prostate and later, transurethral resection of the prostate was the popular treatment for BPH. Nowadays medical therapy that involves the use of alpha-adrenergic antagonists, 5 alpha-reductase inhibitors, antimuscarinics, beta-adrenergic agonists, phosphodiesterase type 5 inhibitors, vasopressin analogs, and phototherapeutic are more popular.
In India, Herbal medicines are considered safer than synthetic medicines for the treatment of mild to moderate conditions of BPH. Crenilton, one such medicine prepared from rye grass pollen extract is a registered pharmaceutical product in Western Europe, Japan, Korea, and Argentina. Homeopathy, Ayurveda, and Unani systems do offer alternatives to reduce symptoms and improve quality of life (QoL) in BPH patients. However, despite the promising benefits of the alternative a complete scientific validation is still lacking.
Proton beam therapy (PBT) is an advanced form of radiotherapy, with radiation treatment delivered by accelerated proton beams rather than X-rays. A proton beams very little radiation beyond the edge of the tumor being treated.
Recent advances in BHP management
i) Water ablation: Water ablation is a new treatment for prostate enlargement in recent years. There are 2 types of water ablation procedures. First, water is injected into the prostate using a probe passed up the urethra and the pressure of the water is then used to destroy some of the prostate tissue, making it smaller. The second type is similar, but steam is used in place of water, to destroy prostate tissue [9]. Water ablation has fewer side effects than transurethral resection of the prostate.
ii) Rejuvenate the prostate/Embolization technique: This therapy has been tried in 14 men and in 13 it was successful in New Orleans, USA. The biggest advantage was none of them suffered from the most feared complications for prostate treatments-namely impotence, incontinence, or infection. The technique involves introducing a catheter through the femoral artery that travels until it reaches the prostate artery. Once there, microspheres are released that obstruct this blood vessel and prevent the passage of nutrients that feed the gland. By doing so the prostate stops growing abnormally and ends the annoying urinary symptoms. The procedure is minimally invasive and is performed under local anesthesia and on an outpatient basis, therefore there is no need for hospitalization as the treated patients were able to leave the hospital the same day as the intervention [16].
The management of BHP in our study included medical treatment in 54 (80%) persons, remaining 12 (20%) surgical interventions and for Cancer Prostate 2 person had only surgery, another 2 had surgery followed by Chemotherapy 3 persons had the surgery, chemotherapy, and Hormone/immunotherapy.
Outcomes
The outlook for benign prostatic hyperplasia is good, although it can cause significant discomfort. As the prostate gland grows, symptoms may become worse, warranting medication or surgery. Delay in treatment can cause lasting bladder damage that can’t be treated. With increased life expectancy, BPH is going to be the most prevalent disease in the aging male and the incidence of symptomatic disease will also increase in the millennium. BHP cases after the treatment are leading almost a normal life in our group.
It is reported that 100% of men who have early-stage prostate cancer will survive more than 5 years, but in practice, the diagnosis is delayed and about one-third only will survive for 5 years after diagnosis. Men with advanced prostate cancer or whose cancer has spread to other regions have lesser survival rates as was in the case of our friend, who survived for just 2 years despite the best possible treatment in India and the USA. Studies in the USA of late indicate that during 2010-2017, the incidence of T1a/b prostate cancer has remained stable, but clinically significant T1a/b disease has increased over that time, from 38.8% in 2010 to 44.1% in 2017 (p < .001). Similarly, the chance of being diagnosed with T1a/b non-clinically significant disease decreased from 61.3% in 2010 to 55.9% in 2017.
Role of preventive medicine in prostate health
1. Sleep: Sleep is essential for the health of the reproductive organs and the production of sex hormones. Sleeping less than recommended decreases testosterone and increases stress hormones in the body of men. Poor sleep habits can cause changes in blood sugar levels, which are linked to prostate enlargement.
2. Consumption of antioxidants: Removing toxins is essential for prostate health, and Phytochemicals are antioxidants created by nature that have a detoxifying effect on the human body. Therefore, it is recommended to consume drinks rich in antioxidants, like hibiscus, green, and ginger tea, every day.
3. Ensure vitamin D levels: Vitamin D levels less than 60 ng/ml, affect the production of testosterone. And a decrease in testosterone, the prostate increases in size to compensate. Vitamin D can be obtained by exposure to sunlight regularly for at least 3 days a week without sunscreen. The conversion of 7-DHC to previtamin D3 and its photoproducts and formation of previtamin D3 and vitamin D3 is maximal between 11 a.m. to 2 p.m. of the day during the entire year [12]. Alternately vitamin D3 supplements (60,000 IU) can be taken.
4. Use only natural cleaning products: Household chemicals like deodorants, shampoos and household cleaners, contain Xenoestrogens that are harmful to Prostate health be avoided and use natural cleaning products.
5. Anti-inflammatory diet: High-quality fats and unsaturated fatty acids found in avocados, olives, olive oil, fish, and coconut oil and butter from the milk of organically raised cows are essential for testosterone production and a healthy prostate. Pomegranate polyphenols inhibit the proliferation of cancer cells by regulating genes that affect androgen synthesis. In juice or dry extract, 2 - 3 glasses or 400 mg - 800 mg per day.
6. Accelerate intestinal peristalsis: A plant-based diet rich in fiber not only has an anti-inflammatory effect but also helps to eliminate toxins from the body faster as they increase rapid intestinal peristalsis. Thus, chia seeds, fermented foods, foods containing probiotics, and animal bone broths increase Intestinal permeability and facilitate the removal of food residues from the intestines faster.
7. Fasting: Fasting is one of the best and easiest ways to increase testosterone levels, reduce systemic inflammation and inhibit cancer formation. Depending on how you eat over 24 hrs. there should be at least 4 pm between dinner and breakfast. Ideally eating during the 8 hours of the day- from 11 am to 7 pm, is the best and a break of 24 hours fortnightly (the concept of Ekadashi in Indian culture) is the easiest way.
8. Pranayama: One of the most popular and simple stress management practices is deep breathing exercises known as Pranayama in Yoga, which calm the sympathetic nervous system, responsible for the so-called “fight or flight” instincts and help to relax.
9. Ensure adequate Microelements: Microelements Zinc and magnesium stimulate testosterone production and help to remove xenoestrogens from the body. They with selenium, strengthen immunity and help the body fight toxins. Magnesium is found in pumpkin seeds. Green smoothies, GLVs, and healthy organic meat.
10. Role of high-quality omega 3 supplements: Omega3 suppresses prostate inflammation and stimulates testosterone production. Additional consumption of 200 - 500 gamma-linolenic acid prevents inflammation.
11. Other beneficial substances for Prostate health: Additional vitamins K2, probiotics, and anti-inflammatory plant compounds - resveratrol, pterostilbene found in blueberries and green tea, to boost immunity and act as antioxidants.
12. Diet can Determine the risk: To preserve men’s health, you should eat moderately or completely avoid fatty (bacon, fatty meat, sour cream, butter, sausage), spicy (flavored with mustard, pepper, horseradish) food. When the human body reacts to coffee, beer, and strong alcoholic drinks, more blood enters the prostate, and it enlarges, therefore moderate consumption is advised. Better to drink green tea, eat more Tomatoes, Salmon, watermelons, Berries (Strawberries, blueberries, raspberries, and blackberries) soya products, cabbage, Broccoli, Nuts, vegetables -onion and Garlic and fish, grapefruits, Citrous fruits like Oranges, lemon, Amla in whom the provitamin lycopene is found, that protects the body’s cells from the harmful effects of the environment [13].
13. Promote/use herbal teas: Research has established the positive effects of many plants on men’s health. For the prevention of prostatitis, saw palmetto extract, and nettle stem extract (Churike Gida, Climbing nettle) are effective means of improving prostate function.
14. Drinking water: Water not only cleanses the entire body of toxins but also prevents urine retention, which otherwise could enter the prostate glands reducing the probability of the bacteria causing inflammation of the prostate. Therefore, it is advised that an individual weighing 60 kilograms, must drink almost 2 liters of water every day.
15. Be moving: One of the biggest problems of the modern man is low physical activity. All or most of the day sitting at work will lead to impaired blood flow to pelvic organs. Sedentary work and low physical activity reduce testosterone levels and can even lead to prostate inflammation. Regular physical activity suppresses inflammatory processes and improves prostate health. Better take a walk after sitting in one place for a long time. One must also do pelvic floor exercises like while standing, raise your knees as high as you can toward your stomach, or while lying straight, bend your knees in half and raise your pelvis. Simple exercises like walking, cycling slowly, or playing active games should be done throughout the day.
16. Beware of cold: So, called “Healthy” bathing in cold water or splashing in cold water after heating up in the sauna also harms the prostate. Getting cold or freezing can lead to the development of prostatitis, so it is better to take a hot bath during winter. Use a longer coat or jacket in the cold season if required.
17. Sex for prostatic health: Regular sexual intercourse with a regular partner, during which the drainage of the prostate improves, and reduces the chance of infection. Prostate inflammation can also be caused by bacteria and fungi spread during unsafe sex. Long abstinence is also not good. Therefore, masturbation may be a good option if safe sex is not possible. “Frequent masturbation during men’s 20s and 30s increased their risk of prostate cancer, but men in their 50s who masturbated frequently had decreased risk [14]. Another recent research asking men to answer questions about how often they ejaculated irrespective of how (sex, masturbation, or wet dreams) tracked almost 32,000 of these men for 18 years. They inferred that those guys who did it the most (at least 21 times a month) had about a 20% lower chance of prostate cancer, compared with those who did it less (4 to 7 times a month) across several age groups [15]. Researchers are still studying the connection between ejaculation and prostate health. Doctors may not be ready to write prescriptions for “more Sex!” yet. But since masturbation and safe sex probably won’t cause any health problems, there’s likely no harm in doing them more often.
18. Other lifestyle changes: Some strategies that may ease BPH symptoms include- Managing stress, quitting smoking, avoiding fluids at the night to reduce night-time urination, practicing bladder training exercises, emptying the bladder when urinating, avoiding medications like antihistamines, diuretics and decongestants, if possible, limiting fluid intake to 2 liters of liquids each day.
If these lifestyle changes are not effective, medication or surgery are recommended.
Takeaway message
U+027A3 Treating BPH can range from making simple lifestyle and dietary changes at home to medication and surgery.
U+027A3 Reducing red meat consumption and eating plenty of fruits and vegetables can help manage symptoms.
U+027A3 If the doctor suggests a “watch and waits” approach, stay in touch with your doctor about symptoms.
U+027A3 If the suggested lifestyle changes are not effective in reducing the symptoms, more aggressive treatment may be needed.
U+027A3 Prostate cancers are showing a significant increase in incidence along with mouth and kidney among the male population and lung cancers globally. Data regarding the true incidence of prostate cancer in India is limited.
U+027A3 Prostate cancer in India can be treated by Immunotherapy at eight Cancer Healer Centres across the country, with a 10-year relative survival rate of 98%. The therapy enhances the body’s immune system and is a surgery-free cure for prostate cancer.
- Bhat SA, Rather SA, Islam N. An overview of benign prostatic hyperplasia and its appreciation in Greco-Arab (Unani) system of medicine. Asian J Urol. 2022 Apr;9(2):109-118. doi: 10.1016/j.ajur.2021.05.008. Epub 2021 May 29. PMID: 35509487; PMCID: PMC9051355.
- McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, Lepor H, McVary KT, Nyberg LM Jr, Clarke HS, Crawford ED, Diokno A, Foley JP, Foster HE, Jacobs SC, Kaplan SA, Kreder KJ, Lieber MM, Lucia MS, Miller GJ, Menon M, Milam DF, Ramsdell JW, Schenkman NS, Slawin KM, Smith JA; Medical Therapy of Prostatic Symptoms (MTOPS) Research Group. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003 Dec 18;349(25):2387-98. doi: 10.1056/NEJMoa030656. PMID: 14681504.
- Hariharan K, Padmanabha V. Demography and disease characteristics of prostate cancer in India. Indian J Urol. 2016 Apr-Jun;32(2):103-8. doi: 10.4103/0970-1591.174774. PMID: 27127351; PMCID: PMC4831497.
- Jain S. Epidemiology of prostate cancer in India. December 2014Meta Gene 2(C):596-605.
- Hashmi A. Prostate Cancer Cases Are Growing More Serious. https://www.medscape.com/viewarticle, 07 July, 2022
- Prostate enlargement. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases
- Thakur V, Singh PP, Talwar M, Mukherjee U. Utility of free/total prostate specific antigen (f/t PSA) ratio in diagnosis of prostate carcinoma. Dis Markers. 2003-2004;19(6):287-92. doi: 10.1155/2004/913870. PMID: 15258330; PMCID: PMC3851065.
- Malati T. Prostate specific antigen in patients of normal, benign prostate hypertrophy and carcinoma prostate. Indian J Clin Biochem. 2006; 21:34–40.
- Treatment of Benign prostate enlargement. https://www.nhs.uk/ conditions/ prostate-enlargement/treatment/
- Harinarayan CV, Holick MF, Prasad UV, Vani PS, Himabindu G. Vitamin D status and sun exposure in India. Dermatoendocrinol. 2013 Jan 1;5(1):130-41. doi: 10.4161/derm.23873. PMID: 24494046; PMCID: PMC3897581.
- Enlarged prostate diet: Foods to eat and avoid. https://www.medicalnewstoday.com/articles/321079
- Masturbation Frequency Linked to Prostate Risk in 20s, Protection in 50s. By Daniel J. DeNoon, medically Reviewed by Louise Chang, MD 27 January 2009, https://www.webmd.com/prostate-cancer/news/20090127
- Can Sex, Masturbation Affect Prostate Cancer Risk? R. Morgan Griffin and Medically Reviewed by Dany Paul Baby, MD on 22 April 2022, https://www.webmd.com/prostate-cancer/
- McVary KT. Management of benign prostatic hyperplasia (BPH). American Urological Association. https://www.auanet.org/guidelines/ 25 Sept. 2017
- Alvarez M. Can enlarged prostate shrink itself? https://www.quora.com/