More Information
Submitted: April 01, 2024 | Approved: April 11, 2024 | Published: April 12, 2024
How to cite this article: Suresh K. Oral Cancer Management is not just Treatment! But also, how early Pre-cancerous Lesions are Diagnosed & Treated!!. Arch Cancer Sci Ther. 2024; 8: 007-012.
DOI: 10.29328/journal.acst.1001039
Copyright License: © 2024 Suresh K. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abbreviations: CT scan: Computerized Tomography Scan; MRI: Magnetic Resonance Imaging; PET scan: Positron Emission Tomography Scan; FNAC: Fine Needle Aspiration Cytology; PICC: Peripherally Inserted Central Catheter; NACT: Neoadjuvant Chemotherapy; DCF: Docetaxel, Cisplatin and 5FU
Oral Cancer Management is not just Treatment! But also, how early Pre-cancerous Lesions are Diagnosed & Treated!!
Suresh Kishanrao*
Public Health Consultant, Bengaluru, India
*Address for Correspondence: Suresh Kishanrao, Public Health Consultant, Bengaluru, India, Email: [email protected]
Oral Cancer (OC) or squamous cell carcinoma of the oral cavity accounts for approximately 3% of all cancers worldwide, with increased incidence in developing countries. The use of tobacco is directly associated with approximately 80% of oral cancers, especially in older men over 40 years of age. As nearly one-third of the Indian population over 15 years consume smokeless tobacco in one or the other forms, a recent increase has been observed in OC incidence among women and young adults. Lately, the sexual behaviors of young & homosexuals have resulted in the emergence of oropharyngeal cancers due to infection with HPV 16.
About 60% of oral cancer cases in India have a five-year survival rate, and this can be improved to 70% to 90% by mere early detection in stages I and II and with various treatment modalities. Despite the well-known benefits of oral cancer screening for the whole population in developing countries remains controversial. It is imperative to address the cultural barriers and societal norms, which limit the acceptability and participation in screening programs in India and many developing countries. This unique challenge of increasing OC morbidity in India and developing countries requires horizontal integration of the health systems with new services focused on cancer control, which gives the best chance for long-term survival, improved outcomes, and affordable care!
This article is based on the author’s experience of overseeing 1 case of early detection and 2 cases of delayed diagnosis, outcomes and relevant literature review, and current guidelines for the management of OC.
Cancer is a non-communicable disease in which cells of any organ of the body grow out of control. Cancer incidence rates are rising at an alarming rate in India and are expected to rise by 12% in the next 5 years [1-6]. Oral Cancer includes cancerous lesions in the oral cavity, the inner lining of the lips and cheeks called buccal mucosa, teeth, gums, the front of the tongue, the floor of the mouth below the tongue, and the hard palate (bony roof of the mouth). Oral cancer is a major problem in India as, its incidence is estimated to be around 150 cases per million population based on around 210,000 new cases of oral cancer reported in 2023 and each year in the country, with men being at higher risk than women [2,3]. Mizoram, Manipur, and Arunachal Pradesh are states with the highest cancer rates in India. Age-adjusted rates of oral cancer in India are high, at 20 per 100,000 population, and account for over 30% of all cancers in the country [3,4]. The variations in incidence & pattern of the disease, are due to the combined effect of an aging population, & regional differences in the prevalence of disease-specific risk factors [2,6].
Oral Cancer (OC) is of significant public health importance to India because i) it is diagnosed at late stages resulting in low treatment outcomes and considerable costs to the patients who cannot afford this type of treatment [1], ii) It’s the insidious onset and slow progress does not threaten the patients to seek urgent consultation iii) In India and other middle- and low-income countries inadequate access to trained providers and limited health services especially rural areas, is the main cause of delay associated with advanced stages at detection time iv) Oral cancer affects those from the lower socioeconomic groups, to higher exposure to risk factors such as the use of tobacco especially non-smoking tobacco like Zarda, Gutka, Beatle nuts, etc., v) Even though the clinical diagnosis is easy via examination of the oral cavity and tongue it’s practice is poor. Risk Factors associated with OC are:
i) Age: Oral cancer is more common in people over 50
ii) Gender: Men are more likely to develop oral cancer than women
iii) Diet: A diet low in fruits and vegetables that increases the risk
iv) Sun exposure: Prolonged exposure to UV radiation of the sun increases the risk of lip cancer
v) Previous cancer treatment: People who have undergone radiation therapy for head and neck cancer have an increased risk of OC.
The only good news about OC is that it has a long natural history, most cases of OC arise from pre-cancerous lesions, allowing curing if diagnosed early, offering the best chance for long-term survival, improving treatment outcomes, and making the care affordable.
Diagnosing oral cancer typically involves:
i) Oral/Dental Examination - The first step is a physical examination, inside the mouth, tongue, gums, and throat for abnormalities, such as lumps, bumps, or discolorations
ii) Biopsy - If any suspicious areas are found, the next step is to perform a biopsy, which involves taking a small tissue sample from the affected area and then sending it to a laboratory for analysis to determine whether it is cancerous and
iii) Imaging Tests: - X-rays, CT (computed tomography) scans, or MRI (magnetic resonance imaging) scans, will help diagnose oral cancer and determine the extent of cancer’s spread.
This article is based on the author’s experience of overseeing 1 case of early detection and 2 cases of delayed diagnosis.
A case from Bhutan with a nonsmoking tobacco chewing habit
In one of my Public Health Consultancy visits in 2008 to Bhutan, the accompanying officer of Govt. Bhutan took me to her village home for lunch on the way to Phuentsholing. After lunch her mother wanted me to check and give an opinion. She was aged about 55 years her main complaint was a light-colored patch for over 6 months inside the mouth, it was painless but not healing despite indigenous and local treatment that involved topical applications and some antibiotics. On examination the oral hygiene was bad as she was used to eating betel leaves with nuts and some local tobacco called Zarda for nearly 10 years 6 - 8 times a day. The entire month was red, but I could see a leukoplakic patch on the upper right buccal cavity.
I suspected it to be precancerous and asked my colleague to take her to Kolkata as soon as promised and get a biopsy done. They did go the very next week, A Biopsy indicated a cancerous lesion, and a surgical excision was done followed by Radiotherapy for 6 sessions fortnightly. She recovered fully and happily, living even now.
A delayed care seeking case from Raichur, Karnataka
Manoj a nephew of mine called early in the morning on 6 November 2023, informing that his mother and my cousin Laxmi, a female aged 60 years, a known diabetic for 20 years, mother of 2 grown-up children, was admitted to a Private Oncology hospital’s Head and Neck Oncology Unit, in Bengaluru on 25 October 2023 and has been diagnosed as having Primary Squamous cell Carcinoma of left buccal mucosa. In short, her main complaint was of a non-healing ulcer in the left side of the mouth above 2nd molar teeth for over 6 months. She consulted a private general doctor, then a Dentist in Raichur district, Karnataka, and a government medical college hospital in Bellary the neighboring district in Karnataka. It was there in July 2023 that for the first time, she was asked to get investigated by biopsy. As her husband was ailing at that time, she postponed her consultation, till she noticed difficulty in opening the mouth and masticating in September 2023. In the meantime, her husband referred her for a consultation in Bengaluru for his Knee joint problems, So, she got checked for her problem in the neighboring facility.
The Head & Neck Oncologist wrote his finding of 25 October 2023 as:
1. Vitals: Conscious level- Alert, Weight= 49 Kg, Fall Score= No risk.
2. Oral cavity: i) Ulcerative growth in left-sided buccal mucosa superior to gingivobuccal sulcus, inferior to lower gingivobuccal sulcus, medially up to gingival mucosa, anteriorly up to 2nd premolar and posteriorly up to retromolar trigone
3. Neck: Left level IB lymph node palpable.
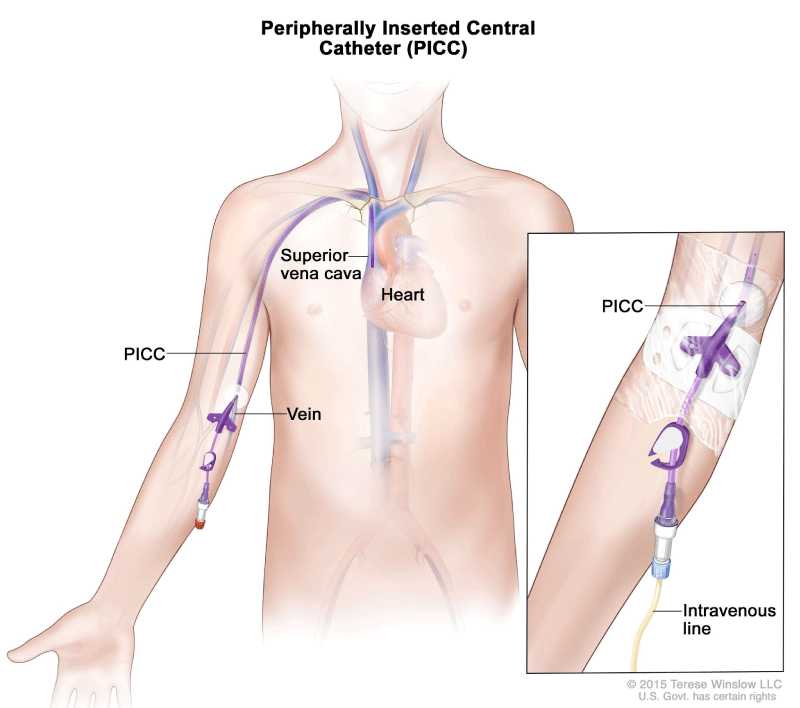
As an investigation routine blood tests, a CT scan of the Head and Neck, and a CT Thorax (basal View) were done, and through them, a provisional diagnosis of CA was done on 31 October 2023. It revealed Small well defined subpleural and peri-pleural nodules bilaterally in the upper and lower lobes, too small to characterize as secondaries, but metastasis could not be ruled out. Therefore, A Peripherally Inserted Central Catheter (PICC) was done which is a thin, flexible tube that is inserted into a vein in the upper arm and guided (threaded) into the superior vena cava above the right side of the heart to used to give intravenous fluids, blood transfusions, chemotherapy, and other drugs on 6th November 2023. Neoadjuvant Chemotherapy (NACT) with DCF regimen in stage III, squamous cell cancer, followed by PET Scan assessment was planned to start after counseling the patient and the accompanying son about the prognosis, lung nodules status, side effects, and future management options. I entered the scene at this stage and discussed it with the medical oncology consultant.
A PET scan report after 2 cycles (28 Oct.23 & 03 Dec 23) report of 16 December 2023 read: Squamous Cell Carcinoma of left retromolar trigone on examination:
1) Oral cavity with proliferative growth of 3 x 3 cm, in left-sided buccal mucosa superior to gingivobuccal sulcus, inferior to lower gingivobuccal sulcus, medially up to gingival mucosa, anteriorly up to 2nd premolar & posteriorly up to retromolar trigone, bleeding on touch, neck nodes not palpable.
2) Whole body images were acquired in 3 D mode 50 minutes after IV injection of 7.8 mCi of 18F-FDG, using a dedicated BGO-PET Scanner. FBS before tracer injection was 89 mg/Dl. Water was used as a negative contrast. Reconstruction of the acquired data was performed to obtain PET CT Scan images in Trans axial, coronal, and sagittal views.
3) The Impression was known case of left premolar trigone status post-chemotherapy.
- Mildly hypermetabolic ill-defined isodense soft tissue density tissue thickening in the left retromolar trigone extending along the lower gingivolabial sulcus adjacent to the left first and second molar teeth suggestive of residual primary tumor.
- No significant FDG avid cervical lymph nodes.
- No other abnormal hypermetabolic lesion in the rest of the body.
21/01/2024: Final diagnosis was Squamous cell carcinoma, left buccal mucosa
After chemotherapy PET scan showed residual primary in the lower gingivobuccal sulcus and 4 mm non-FDG avid nodule in the left lower lobe of the lung and the rest lung field was normal. No uptake anywhere else in the body. The institutional tumor board discussed and decided on surgery given the small resectable primary and good performance status. Planned for follow-up of indeterminate nodule.
Surgical procedure: Composite Resection of left buccal mucosa (left segmental mandibulectomy+ left upper alveolectomy + left masseter+ medial pterygoid removal +left selective neck dissection (I-IV) + Pectoralis major mucocutaneous Flap reconstruction was done under GA on 01/13/2024):
Findings: Ulcerative lesion in left retromolar trigone, approximately 2 x 2 cm, involving both upper and lower gingivobuccal sulcus, anteriorly up to 4cm from labial commissure, posteriorly left retromolar trigone. Suspicious nodes in left level IB.
She was discharged on 01/22/2024 with advice for neck and shoulder exercises, maintaining neck position in flexion, good surgical site care, and oral hygiene, and return after 1 month.
After a month she was put on combined Radiotherapy & Chemotherapy sessions. Radiation is for about 10 minutes daily from Monday to Friday and Chemotherapy once a week. As offend March she is doing fine but for aphthous ulcers, with 3 more radiotherapy left.
A delayed care-seeking case from Bengaluru, Karnataka
This case is the wife of a close friend and resident of our residential complex, who I thought was out of station visiting her son in the USA, saw her in our routine morning Walk after a gap of 3 months, and I was surprised by her covering the face and having wasted at least half what she was a few months ago. On the first day I was not sure if to enquire, but the next day I did intervene and asked the reason. She told me about her Oral Cancer and operation for the same a month ago and was on her way to radiotherapy. She informed me that she had some sort of discomfort in her left upper first and second molar teeth and was finding it difficult to masticate from those teeth 3 months ago. She had been consulting an Orthodontist at our apartment complex for nearly a month who either did not examine her well or missed the clue. After a month of no relief, she consulted in a private Oncology hospital in Bengaluru in early February 2024. Based on Fine Needle Aspiration Cytology (FNAC), a simple, quick, and inexpensive method performed in the outpatient clinic in early cases Squamous cell Carcinoma was suspected and confirmed after biopsy. A CT scan was done that ruled out secondaries anywhere in the body. The left submandibular lymph node was enlarged a bit, but its biopsy did not indicate secondaries. As surgery is the primary treatment option for nonmetastatic OSCC, less invasive curative surgical approaches were taken. Considering that she was at high risk of recurrence, adjuvant treatment using radiation (6 weekly sessions) is now being done.
Indian National Cancer Registry reports reveal that cancer is showing an increasing trend in India, as from 1990 to 2016, the number of new cancer cases and deaths in India has doubled. The same is expected to rise by 31.4% between 2015 to 2025 witnessing a rise to 2.98 million by 2025 from 2.67 million in 2021. The cancer spectrum differs from region to region within the country due to diverse lifestyles. The northern region is found to have the highest cancer burden, followed by the northeast. For example, the cancer incidence rates in Mizoram’s Aizawl district were seven times higher in men and four times higher in women than in Osmanabad and Beed of Maharashtra [6,7].
Oral cancer is the most common cancer in India amongst men (11.28% of all cancers), and the fifth most frequently occurring cancer among women (4.3% of all cancers). The projected burden of cancers among males by the current year (2024) in India is 62,000 for the tongue and 37,000 for the larynx. When oral cancer is diagnosed early, the 5-year survival rate is above 80%, whereas it’s less than 20% - 30% advanced stage of the disease, unfortunately, the majority are detected in advanced stages. Therefore, the urgency for Oral cancer screening and/or detection and treatment at an early stage [6].
The occurrence and distribution of oral cancer based on the analysis of hospital records from registered oncology institutes of South India over three years (2016-18). A total of 156090 various types of cancers were reported. period of three years, almost similar gender distribution was observed, males (n = 78806, 42.99% per lakh) compared to their female counterparts (n = 77284, 42.16% per lakh). Among males’ lung cancer was the most common type with 17709 cases (9.65% per lakh) and among females, breast cancer was the leading cancer type with 22855 total cases (12.46% per lakh). For three years, a total of 21084 records of malignancies in the oral cavity were identified accounting for 13.51% of cases. Among oral cancers, the tongue was the most common site to be involved accounting for 44.22% (2016–2018) cases followed by buccal mucosa (14.69%), least common site to be involved was the lip which accounted for 3.49% of the total oral cancer cases [4].
In a study in Karnataka of 1227 cancer patients records reviewed at the tertiary care hospital about 10% were oral cancers mouth (5.5%), and tongue (5.2%), though Lung (10.5%) was the leading site of cancer among males followed by esophagus (10%) [7].
Epidemiology of cancers in India
The use of tobacco is directly associated with approximately 80% of oral cancers, especially in older men over 40 years of age. Nearly one-third (30%) of the Indian population over 15 years consume tobacco in one or the other forms. Of late increase is observed in OC incidence among women and young adults due to consuming smokeless tobacco. Recent changes in sexual behaviors of young and homosexuals have resulted in the emergence of oral and oropharyngeal due to infection with human papillomavirus, 16, (HPV 16), a sexually transmitted virus [4,6]. In India Cancers of the head and neck region accounted for nearly one-third (31.2%) of the cancers among males. Oral Squamous Cell Carcinoma (OSCC) dominates all the oral cancer cases recognized and has a detectable pre-clinical phase. Tobacco consumption includes smokeless tobacco and betel quid chewing. Smokeless Tobacco (SLT) products like Madhu Chhap, Hans Chhap, and Miraj and Gutkha brands of Khaleej and Rebel are explicitly sold in the Indian tobacco market. The brands of Vimal, Hira, Rajanigandha, and RMD are Pan masala products. The consumption of smokeless tobacco is higher due to the greater social acceptance, curiosity, and culture. About 35% - 40% of tobacco consumption in India is in smokeless tobacco forms, most of which is Nicotiana rustica, while most smoking tobacco is Nicotiana tabacum.
Excessive alcohol consumption, unhygienic oral condition, and sustained viral infections including human papillomavirus, etc. are some other risk factors for OC.
Presenting symptoms: The most common cancer seen in the oral cavity is squamous cell carcinoma. It presents as a painless discolored patch ulcer, mass, or fissure. As the disease advances, patients may have excessive salivation, trismus, and difficulty in chewing, swallowing, or cervical lymphadenopathy. Mouth ulcers that persist for more than three weeks persistent pain in the mouth or a lump or thickening in the cheek are the key symptoms. Other symptoms include a white or red patch on the gums, tongue, tonsil, or lining of the mouth, a sore throat, or a feeling that something is stuck in the throat, difficulty in chewing or swallowing, or in moving the jaw or tongue. Difficulty in tolerating spicy foods, bleeding or numbness of the tongue or other areas of the mouth, swelling of the jaw that causes dentures to fit poorly or become uncomfortable, loosening of the teeth or pain around the teeth or jaw, changes in voice or having speech problem, a lump or mass in the neck, weight loss, constant bad breath, excessive salivation, repeated biting of cheeks because of sharp teeth are other indications to suspect OC [1,3,4,7]
Screening for oral cancer: Visual Screening Involves:
1. Systematic visual and physical examination of the intraoral mucosa under bright light for signs of Oral Potentially Malignant Disorders (OPMDs), as well as early oral cancer
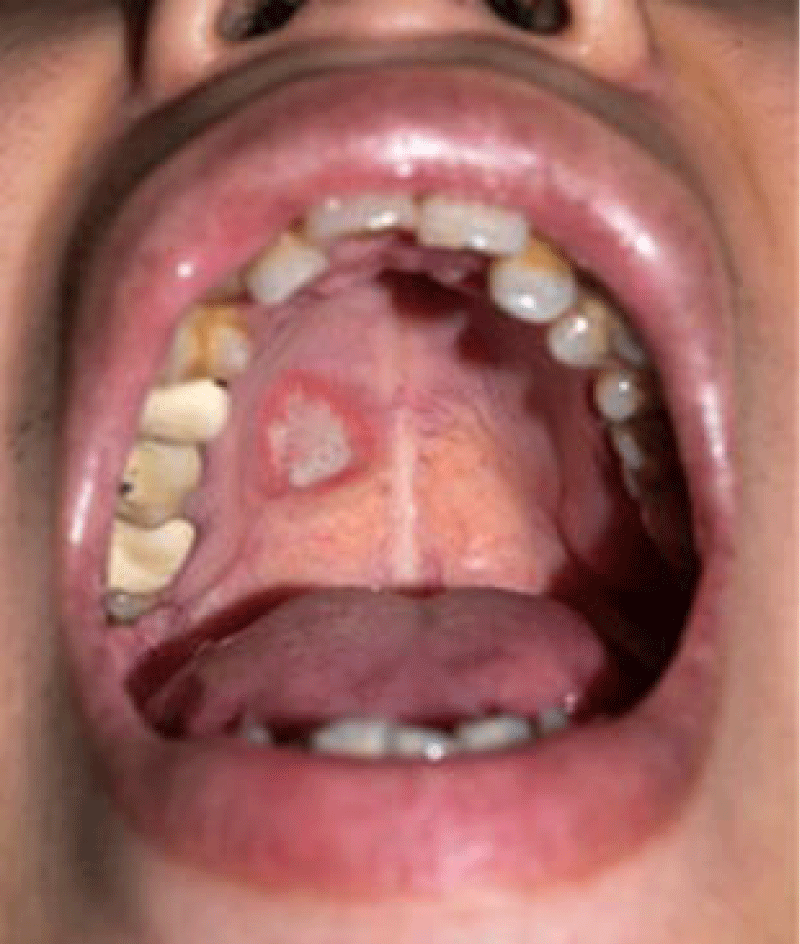
2. Oral visual examination helps to detect different types of oral lesions. Leucoplakia, (Figure 1, source 7), erythroplakia (Figure 2, source 7) palatal changes associated with reverse smoking or beedi smoking and submucous fibrosis all of which are local pre-cancerous.
Figure 1: Homogeneous Leucoplakia.
Figure 2: Erythroplakia.
3. Careful inspection and digital palpation of the neck for any enlarged lymph node.
Management of OSCC: The latest guidelines for the Management of Oral Cavity Squamous Cell Carcinoma (OSCC) recommend a multidisciplinary team approach. Surgery is ideally the primary treatment option for nonmetastatic OSCC as was done in our first case, and less invasive curative surgical approaches are preferred in early-stage disease to minimize surgical-related morbidity. For patients at high risk of recurrence, adjuvant treatment using radiation or chemoradiation is often used as was done in our third case report. Systemic therapy may also be used in the neoadjuvant setting (for advanced-stage disease with the intent of mandibular preservation) or in the palliative setting (for non-salvageable locoregional recurrence and/or distant metastases as was done in our case of Laxmi [8,9]. The practical application of these guidelines leads to,
Sentinel lymph node biopsy-based clinical trials provide evidence for personalized neck management for Oral Cavity Cancer (OCC).
High-dose radiation (with concurrent chemotherapy) for OCC could be a reasonable alternative management strategy to primary surgery when it is not feasible and for patients with early recurrence before the planned postoperative radiation.
Identifying patients with OCC at high-risk Distant Metastases (DM) as was in our second case could allow (1) the risk-adaptive DM screening protocol with the possible local ablative treatment of early-detected oligo-metastases and (2) future evaluation of novel systemic multiagent-regimens-like-Induction chemotherapy, excision of the primary site be used with the aim of mandibular preservation for OCC.
In the adjuvant setting for patients with OCC and high-risk features (positive margin and/or extranodal extension), the standard of care is cisplatin concurrently with radiotherapy. In cisplatin-ineligible patients, docetaxel with postoperative radiation is supported by the best evidence. Other possible options include concurrent cetuximab, carboplatin/5FU, carboplatin/paclitaxel, or the use of accelerated radiation. When improved surgical techniques and peri-operative care in OC is not feasible, In India at least 10 RCTs compared NACT to surgery alone have demonstrated a significant increase in median survival of 17 months in the former, compared to 13 months in the latter. A Prospective non-randomized study during 2007-12, on 20 patients of NACT with DCF (docetaxel 75 mg/m2 day 1, cisplatin 75 mg/m2 day 1, 5-FU 750 mg/m2 per day 1-4) regimen, in stage III Ca have shown clear benefit [7]. Post NACT, Partial response of 58.8%, and a complete pathological response of 17.6% were observed with a response rate of 76.4%. NACT x 3 cycles used. Neoadjuvant Chemotherapy (NACT) with DCF (Docetaxel, Cisplatin, and 5FU) is one of the treatment options that has a survival benefit over DC in oral cancers but it comes at the cost of an increment in acute adverse events [10] (Figure 3.).
Figure 3: Peripherally Inserted Central Catheter [2,10,11].
Oral Cancers are increasing in India and globally. About 60% of oral cancer cases in India and other developing countries have a five-year survival rate, which can be improved to 70% to 90% by mere early detection in stages I and II and treatment, with various treatment modalities. However, the benefits of introducing oral cancer screening for the whole population in developing countries remain controversial.
As it is imperative to address the cultural barriers and societal norms, that limit the acceptability and participation in screening programs. Indian Council for Medical Research (ICMR) has set an example by supporting community-based screening starting with high-risk groups in 2022 and general population in 2023.
This unique challenge of increasing OC morbidity in India and developing countries requires horizontal integration of the health systems with new services focused on cancer control.
- Cancer Burden in India. A Statistical Analysis on Incidence Rates, Shafi, Lubna et.al, Indian Journal of Public Health. Oct–Dec 2023. DOI: 10.4103/ijph.ijph_1587_22
- Oral cancer and its rapid rise in India. https://cytecare.com/blog/head-and-neck/
- Mathur P. Cancer Statistics. 2020. National Cancer Registry Program, India. https://ascopubs.org/doi/10.1200/GO.20.00122
- Asmin PK, Nusrath F, Divakar DD. Occurrence and Distribution of Cancers with Emphasis Upon Oral Cancers in Registered Oncology Institutes of South India - A Retrospective Study. Indian J Community Med. 2024 Jan-Feb;49(1):120-130. doi: 10.4103/ijcm.ijcm_106_23. Epub 2024 Jan 12. PMID: 38425965; PMCID: PMC10900442.
- Top 10 Cancer States in India. 2023 Cancer Statistics in India. drarvindkumar.com https:// /blog/01/11/2024
- Prasad JB. A new approach for measuring incidence cases for India and its States – Till 202520. J Cancer Policy. 2018; 16:57–62.
- Suresh K. Oral Cancer Screening through Accredited Social Health Activists. Biomed J Sci & Tech Res. 50(5)-2023. BJSTR.MS.ID.00801 06/05/2023
- Somashekhar SP. Neoadjuvant chemotherapy (NACT) with DCF regimen in stage III, squamous cell cancer. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2012.30.15_suppl.e147
- India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India: The Global Burden of Disease Study 1990-2016. Lancet Oncol. 2018 Oct;19(10):1289-1306. doi: 10.1016/S1470-2045(18)30447-9. Epub 2018 Sep 12. Erratum in: Lancet Oncol. 2018 Oct 3; PMID: 30219626; PMCID: PMC6167407.
- Mohamad I, Glaun MDE, Prabhash K, Busheri A, Lai SY, Noronha V, Hosni A. Current Treatment Strategies and Risk Stratification for Oral Carcinoma. Am Soc Clin Oncol Educ Book. 2023 May;43:e389810. doi: 10.1200/EDBK_389810. PMID: 37200591.
- Marcus F, Leonardo T, Giani S, Vivian C, Sangia S, Monique C, GuilhermeIglezia S, Delio M, Elisa P, Pietro D, Carlos M, Ana R, Georgia P, Regilane S, Rogerio S, Thiago B. Differences between the use of a central venous catheter and a central venous catheter peripheral insertion: advantages, disadvantages and risk factors associated with each procedure. International Journal of Advanced Research. 2023; 11:761-768. 10.21474/IJAR01/17283.